Author(s): Wildgruber, Moritz
Author(s): Wildgruber, Moritz
11-month-old infant with hard palpable tumor on the right upper arm. Reddish-livid discoloration of the skin. Over the discolored areas tense, edematous as well as overheated tissue. No significant tenderness of the lesion. Threefold circumferential increase of the arm compared to that of the healthy opposite side. Laboratory examination showed thrombocytopenia (76,000/µl), simultaneously elevated D-dimers (5549 ng/ml ) and decreased fibrinogen (189 mg/dl ) as signs of a mild Kasabach-Merritt phenomenon.

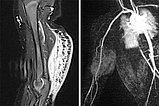
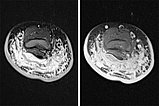
MRI imaging (left – TIRM sequence, right – dynamic MR angiography). In TIRM increased signal of the tumor at the dorsal upper arm. Hyperintense septa perpendicular to the skin, corresponding to extensive local lymphedema. In dynamic MR angiography, the tumor is hyperperfused in the arterial contrast phase with clearly identifiable arterial feeder vessels from the brachial artery.
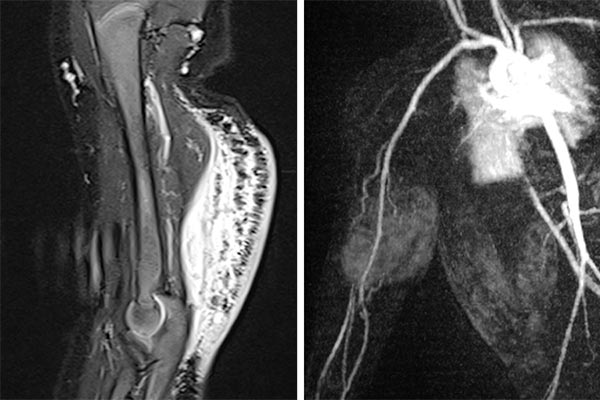
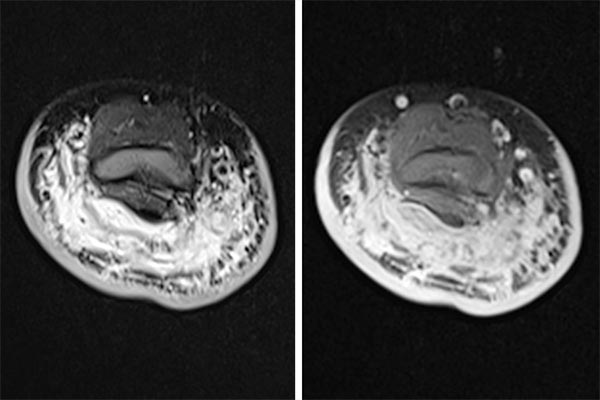
MRI imaging (left TIRM sequence, right T1-weighted sequence with spectral fat saturation after gadolinium administration). Diffuse infiltration of the dorsal upper arm with characteristic thickening of the cutis, subcutaneously pronounced lymphedema as well as diffuse contrast enhancement of the tumor, which are difficult to differentiate from each other. A diagnosis of kaposiform hemangioendothelioma was made on the basis of laboratory examination, clinical findings, and MR imaging.
In view of progressive thrombocytopenia with Kasabach-Merritt phenomenon, the decision was made to perform embolization with biopsy in the same session. To reduce platelet aggregation within the lesion and thus counteract consumptive coagulopathy, oral therapy with acetylsalicylic acid was started concurrently with embolization.
Digital subtraction angiography via the brachial artery (left) and via the microcatheter (right), which was selectively placed in the hypertrophied feeder artery in the right upper arm.
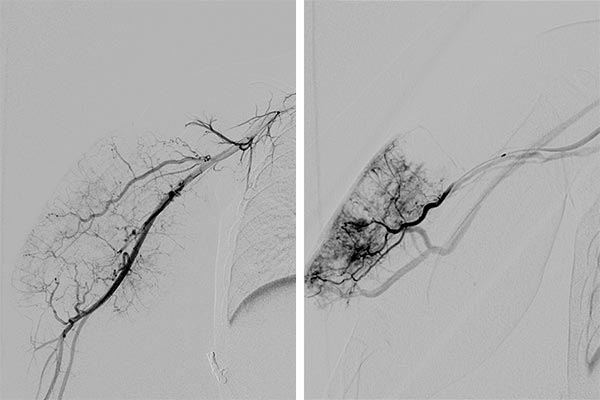
Digital subtraction angiography after embolization with ethylene-vinyl alcohol copolymer via a microcatheter with detachable tip. Simultaneous acquisition of a punch biopsy for histologic examination.

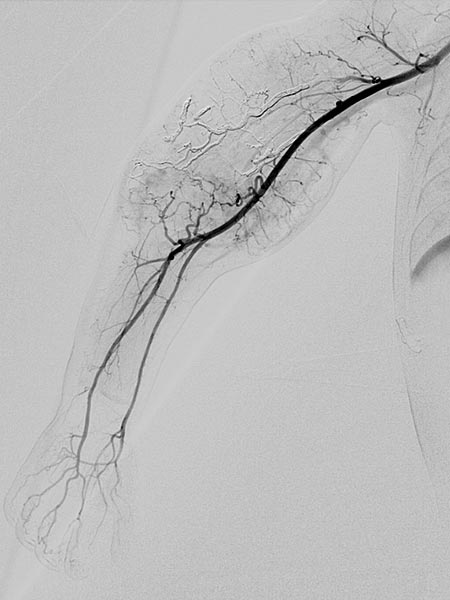
Digital subtraction angiography after embolization of an estimated 70% of the arterial tumor supply to improve the Kasabach-Merritt phenomenon.
Subsequently, initiation of oral therapy with sirolimus. Therapeutic goal: blood level measured in the morning before taking the first medication at about 5–8 nanograms/ml. For this purpose, initially daily, later bi-weekly blood level measurements are required, but these can be performed on an outpatient basis.
Clinical findings over the course of 2 days after embolization (left), 2 weeks after embolization (middle), and 4 months (right) after embolization and start of sirolimus therapy. The arm circumference was now only 4 cm more on the right side compared to the healthy opposite side. Thrombocytopenia had completely normalized within 4 weeks, as had D-dimer and fibrinogen levels. The Kasabach-Merritt phenomenon had completely disappeared. ASA was continued for 6 months in parallel with oral sirolimus therapy.

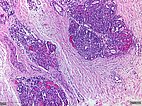
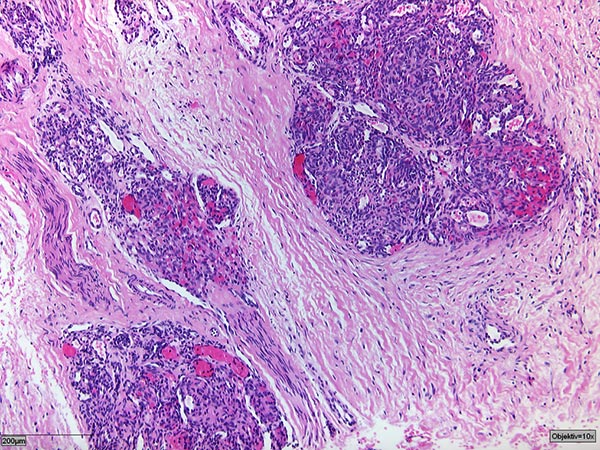
Histopathologic specimen in hematoxylin & eosin stain.
The tumor consists of irregular glomeruloid vascular nodules diffusely infiltrating the soft tissue in a “cannon-ball” fashion. There is an associated stromal desmoplasia.
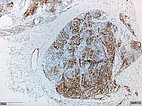
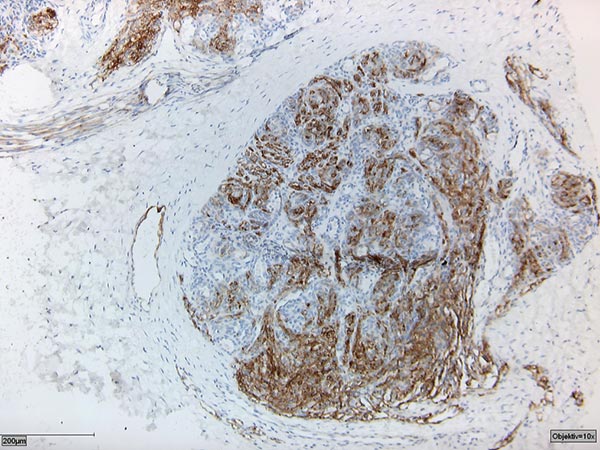
Histopathologic specimen in podoplanin stain (D2-40).
The D2-40 positivity for lymphatic endothelium together with the appearance of a vascular tumor confirmed the diagnosis of kaposiform hemangioendothelioma.
Kaposiform hemangioendothelioma (KHE) is a very rare vascular tumor of infants and young children that often occurs during or after birth. While the tumor has virtually no metastatic potential, it invasively penetrates all tissue layers. KHEs are always extremely hypervascularized and exhibit marked neoangiogenesis of blood and lymphatic vessels. The activated endothelium within the tumor leads to local coagulation activation within the tumor and consequently to a specific form of consumptive coagulopathy (Kasabach-Merritt phenomenon) with characteristic deep thrombocytopenia. The thrombocytopenia can cause life-threatening bleeding, so that rapid therapy is required. Blood transfusions or the administration of platelet concentrates have no lasting effect, as the administered blood products are rapidly activated and consumed within the lesion. Embolization therapy can reduce the contact between the blood and the pathologically activated endothelium and thus primarily treat the Kasabach-Merritt phenomenon. Because of the typical activation of the PI3K/AKT/mTOR signal transduction cascade, sirolimus therapy can significantly reduce tumor growth and curb vascular proliferation. However, this is off-label use, the scientific evidence to date for such therapy is limited and it should be reserved for use in a center.
Published: 2018
All images © Wildgruber