Author(s): Wildgruber, Moritz
Author(s): Wildgruber, Moritz
58-year-old female patient with venous malformation (VM) progressing over years after partial surgical resection in early adulthood. The lesion is visible as a slightly bluish discolored swelling. After initial resection, there had been a postoperative improvement in pain symptoms for over a year. Then the lesion had slowly increased in size again and became increasingly painful due to recurrent thrombophlebitis in the venous malformation.

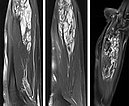
MRI of the forearm in T2-weighted images with spectral fat saturation (left, middle). The characteristically hyperintense, dilated venous convolutes are shown. These lesions enhance contrast medium in the late phase (T1 after contrast; right). The central thromboses appear within these caverns as hypointense areas.
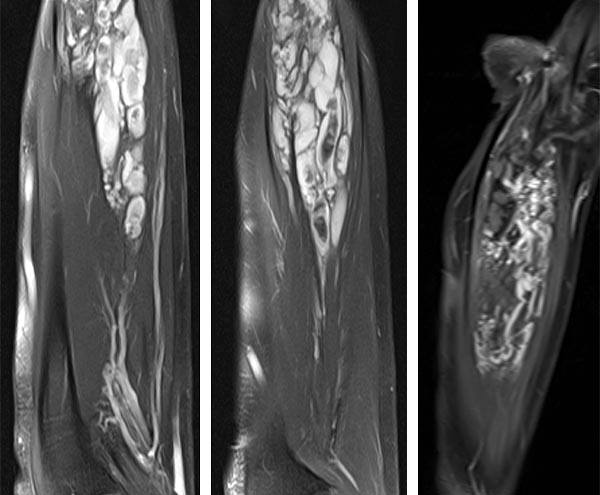
A total of seven sessions of sclerotherapy were performed, in which the venous malformation was sclerosed using polidocanol 3% (up to 4 ml per session). During this procedure, the perfused portions of the malformation are directly punctured with a 21G needle under ultrasound guidance. After aspiration of venous blood, contrast injection is performed to assess the distribution, or rather the communications of the individual malformation portions with draining outflow veins. This is followed by slow injection of foamed polidocanol, followed by elastic compression bandaging for 24 h.
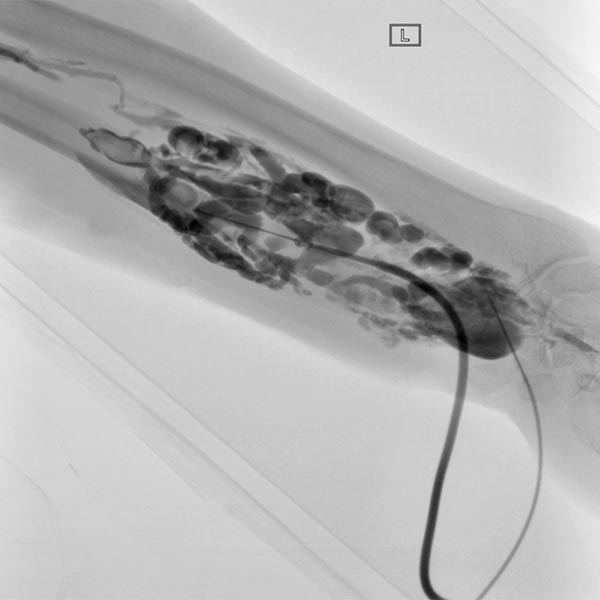
Duplex sonography after multiple sclerotherapy sessions shows almost complete occlusion of the dysplastic venous channels. No more color signals in the now echogenic lesion showing no more open dysplastic venous channels.
MRI of the forearm (T1 with spectral fat saturation after gadolinium administration) demonstrates almost complete occlusion of the dysplastic veins, which initially thrombosed and then subsequently scarred after sclerotherapy.

The patient with the venous malformation (VM) treated here shows a typical clinic course with an equally characteristic medical history. Primary surgical partial resections of vascular malformations usually lead to recurrence if they are incomplete, as was the case here. Slow progression over years to decades is also typical of vascular malformations that never resolve on their own. In the case described, adequate therapy had not been provided for years, which almost led to occupational disability because of the equally slowly progressive symptoms with pain and functional limitation. After successful sclerotherapy, the patient is now back at her job as an office worker and reports only occasional mild pain symptoms.
Annual check-ups and follow-up if symptoms recur have been agreed with the patient, as recurrence can still occur after sclerotherapy.
Published: 2018
All images © Wildgruber