Author(s): Wohlgemuth, Walter A.
Author(s): Wohlgemuth, Walter A.
Immediately after birth, there was a deep dark-red, indistinctly demarcated tumor on the right flank of the body close to the buttocks. From the beginning hemorrhages into the surrounding area were present, visible as hematomas of varying color intensity. Laboratory findings showed massive thrombocytopenia, fibrinogen not measurably low. Constellation of a Kasabach-Merritt phenomenon.

Due to the coagulation failure in the context of the Kasabach-Merritt phenomenon, new and circumscribed hemorrhages developed spontaneously during the first days of life, visible here from different-colored hematomas and small petechial skin hemorrhages.

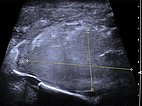
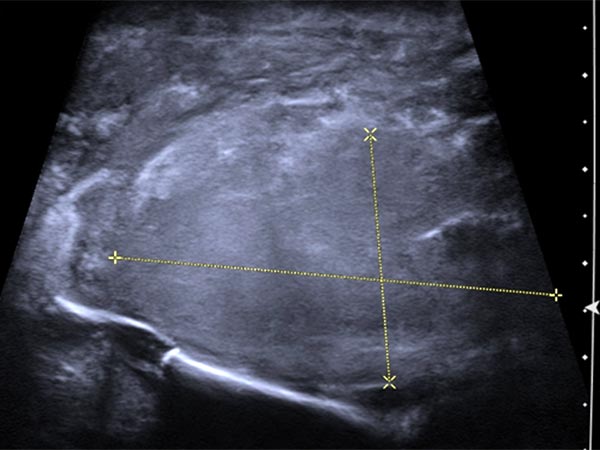
Sonographically, the main subcutaneous extent of the tumor is seen in the depth of the buttock on the right side. The tumor is echogenic, but overall very inhomogeneous and extends to the pelvic bone.
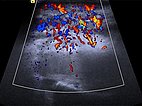
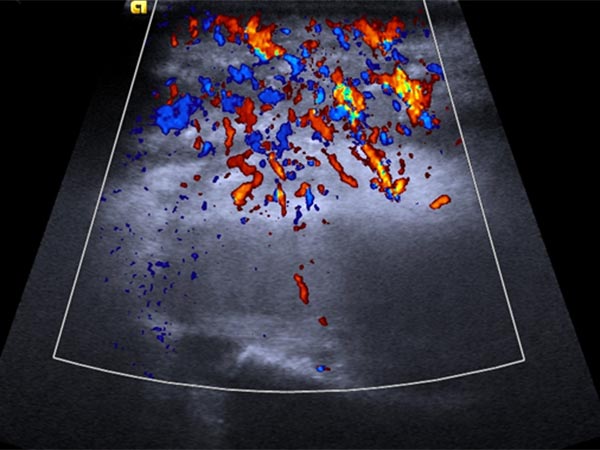
In color-coded duplex sonography the tumor shows marked perfusion. The suspicion of a vascular tumor is thus substantiated.
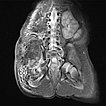
Native T1-weighted MRI shows the tumor to be hypointense. The tumor has blurred margins. The surrounding adipose tissue is saturated with lymphedema.
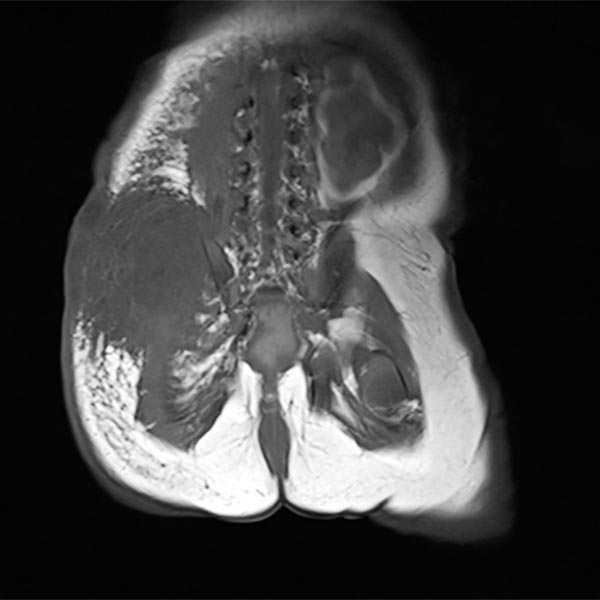
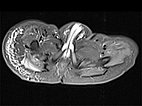
In corresponding T2-weighted, fat-saturated MRI, the tumor shows hypointense parts (hemorrhages), but also hyperintense parts and is overall very inhomogeneous and blurred. The surrounding fat tissue is saturated with lymphedema.
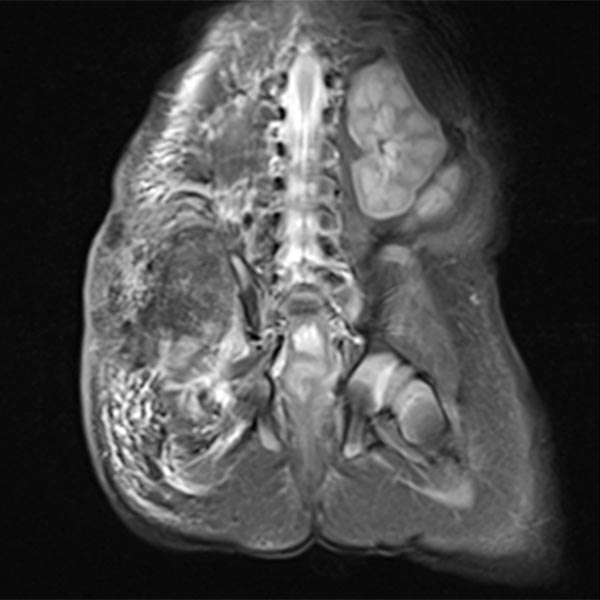
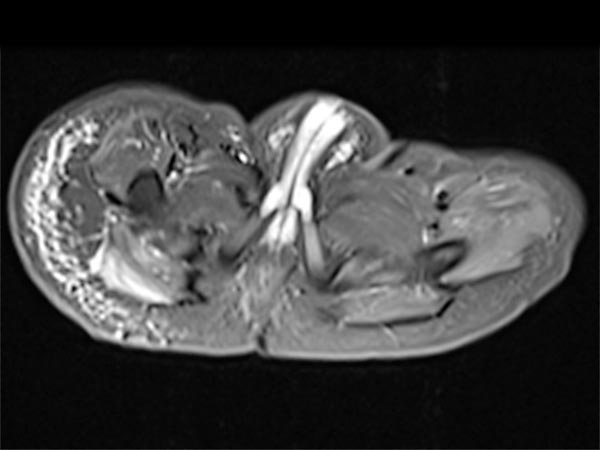
This surrounding subcutaneous lymphedema (hyperintense in axial T2-weighted, fat-saturated MRI ) is a typical feature of kaposiform hemangioendothelioma and also extends significantly in the surrounding area.
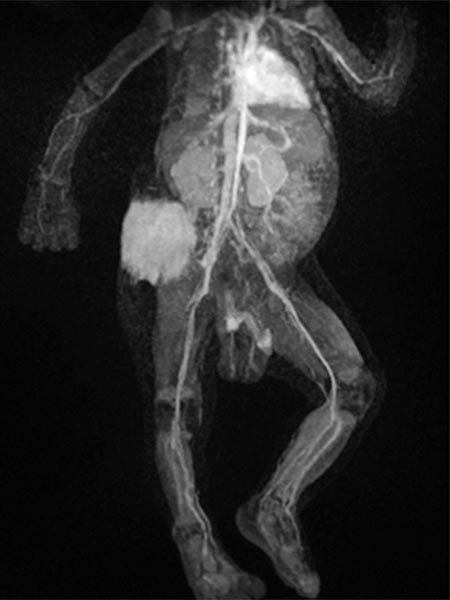
Dynamic contrast-enhanced MR angiography.
Starting in the early arterial phase, the tumor enhances intensively, although not completely.

Dynamic contrast-enhanced MR angiography.
The venous phase shows intense, homogeneous enhancement without immediate direct venous outflow.

Dynamic contrast-enhanced MR angiography.
In the late phase, the highly vascularized tumor continues to show strong enhancement without wash-out phenomenon.
In coronal plane T1-weighted, fat-suppressed MRI after contrast administration, the tumor accumulates contrast strongly. The combination of the clinical picture with vascular, reddish-blue tumor immediately after birth, Kasabach-Merritt phenomenon and typical imaging suggests that the diagnosis of kaposiform hemangioendothelioma is very likely.

In view of massive coagulopathy prohibiting open surgery in this location and lack of improvement with drug therapy and replacement of platelets and coagulants alone, the decision was made to embolize the hypervascularized tumor. Digital subtraction angiography (DSA) shows the highly vascularized tumor supplied mainly from the right superior gluteal artery.
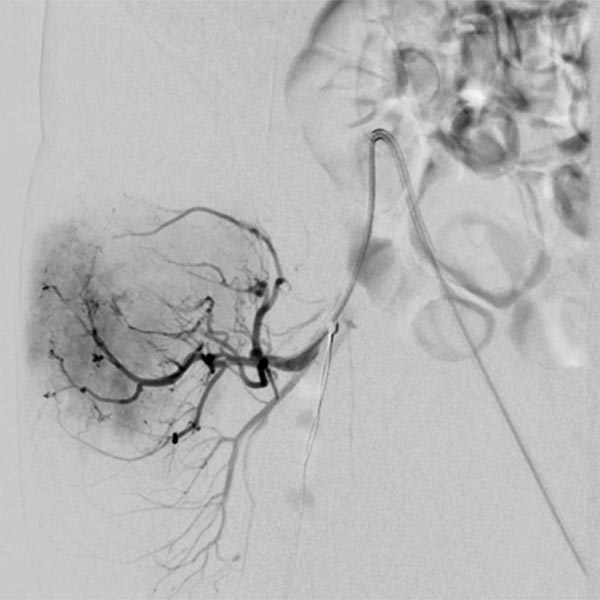
The tumor shows the typical tumor blush with diffuse, strong contrast enhancement on DSA after super-selective catheterization with the microcatheter.
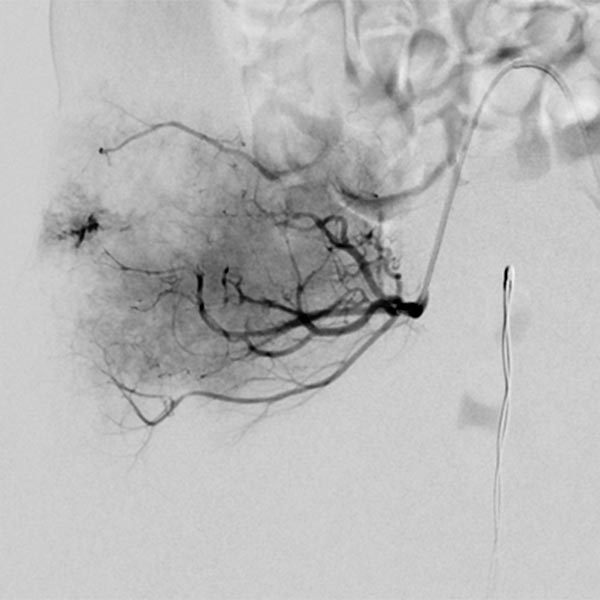
Via the microcatheter, the tumor is now gradually embolized super-selectively with particles 150 microns in size via the supplying arterial branches.
In the control DSA, the main part of the tumor has now been successfully embolized and cut off from the circulation. Only very cranial tumor-supplying branches remained at this stage of the embolization.
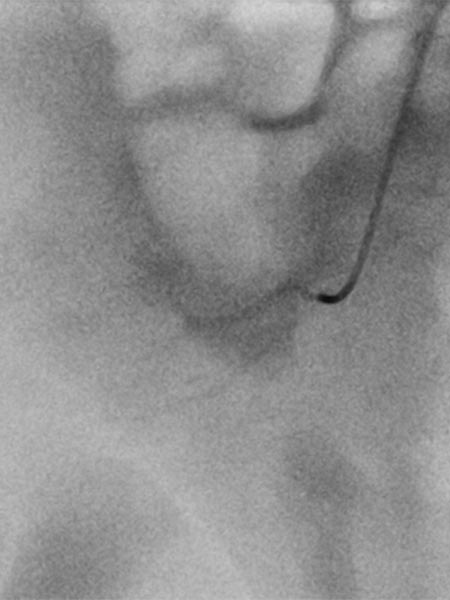
These very cranial parts are now also catheterized super-selectively with the microcatheter and embolized with particles. For better navigation of the microcatheter, the vessels from a previous injection are electronically overlaid by the computer (so-called “overlay display”, white in the image).

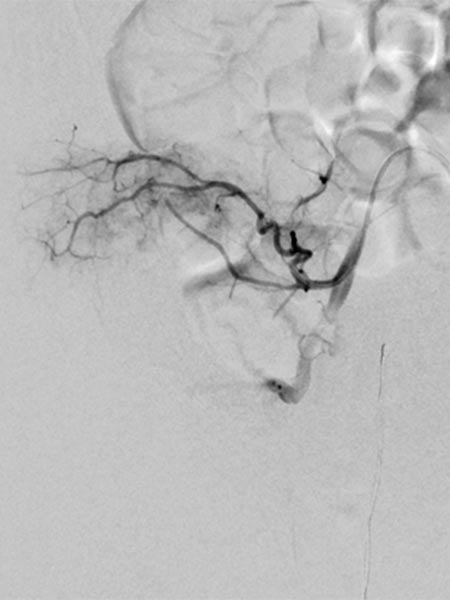
In the final control angiography with long series after injection into the right common iliac artery, the tumor is completely devascularized. The unaffected, physiological arterial branches of the surrounding tissue are all preserved. Thus, the tumor is completely eliminated from the circulation. Activation of coagulation and consumption of platelets in the tumor has stopped.

The clinical course was very encouraging. The volume of the tumor had already decreased immediately after embolization. Platelet levels rose rapidly, as did fibrinogen and coagulation factors. The Kasabach-Merritt phenomenon was suspended. This image 17 days after embolization shows the clinical success.

The typical clinical picture of a newborn with a reddish-bluish tumor immediately after birth, massive coagulopathy with spontaneous hemorrhage and marked thrombocytopenia is clearly indicative of a kaposiform hemangioendothelioma with Kasabach-Merritt phenomenon. In this case, mere substitution of platelets and coagulation factors is usually insufficient. Super-selective embolization while preserving the healthy arteries prevents intratumoral activation of coagulation and trapping of platelets across the massively perfused tumor. This was also very successful in this infant. Currently, the patient is on sirolimus and is developing very well without recurrence.
Published: 2018
All images © Wohlgemuth