Author(s): Wohlgemuth, Walter A.
Author(s): Wohlgemuth, Walter A.
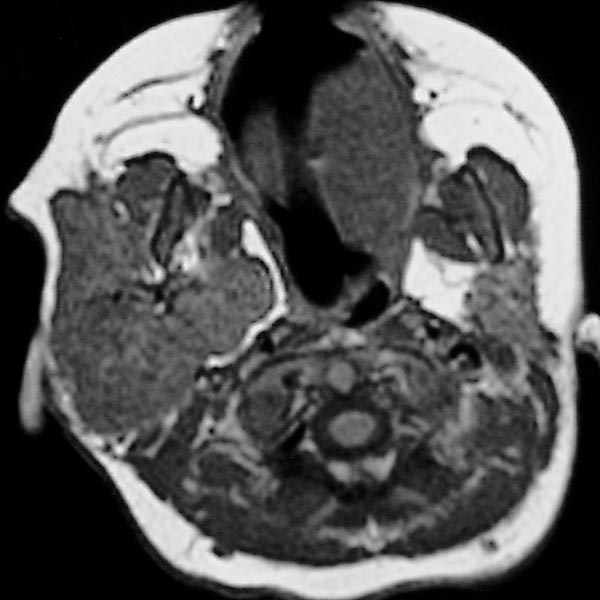
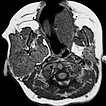
Transverse T1-weighted, non-enhanced MRI of the upper neck shows the tumor to be subcutaneously located, clearly solid, and sharply demarcated from surrounding tissue. The girl is now 12 months old, and the tumor has not regressed.
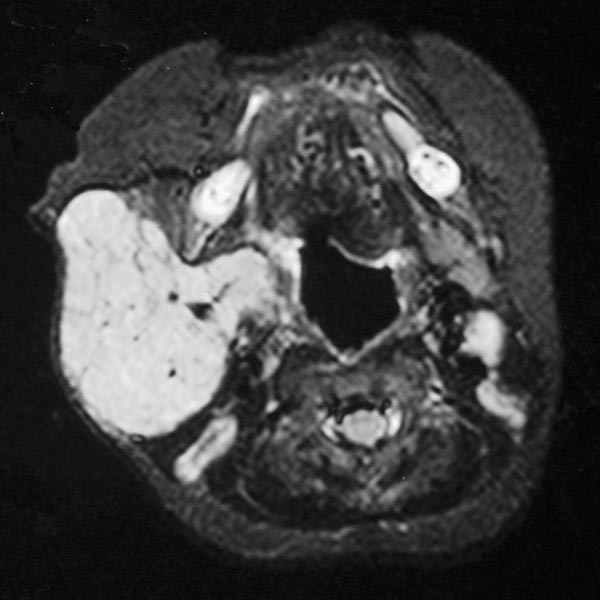
Transverse, T2-weighted, fat-saturated MRI of the upper neck again shows the subcutaneously located tumor very clearly as a hyperintense, sharply demarcated mass with central flow voids as a sign of intense arterial perfusion. Typical image of a subcutaneously located infantile hemangioma.
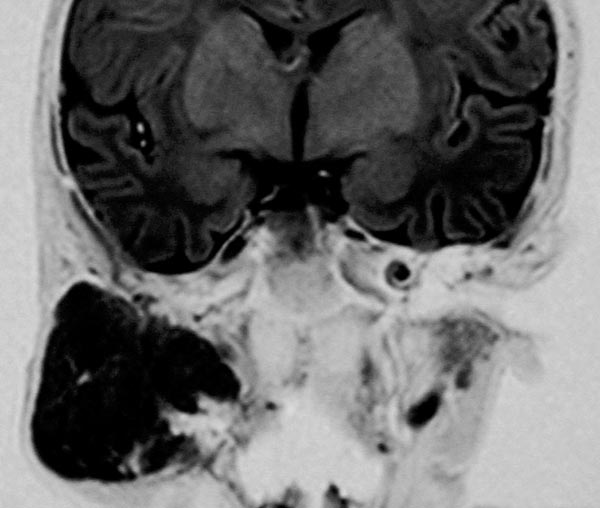
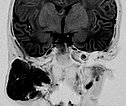
Coronal inversion recovery sequence (MRI) again shows the extent of the hemangioma very clearly. The signal intensity is isointense to the brain tissue. It is clearly a solid mass.
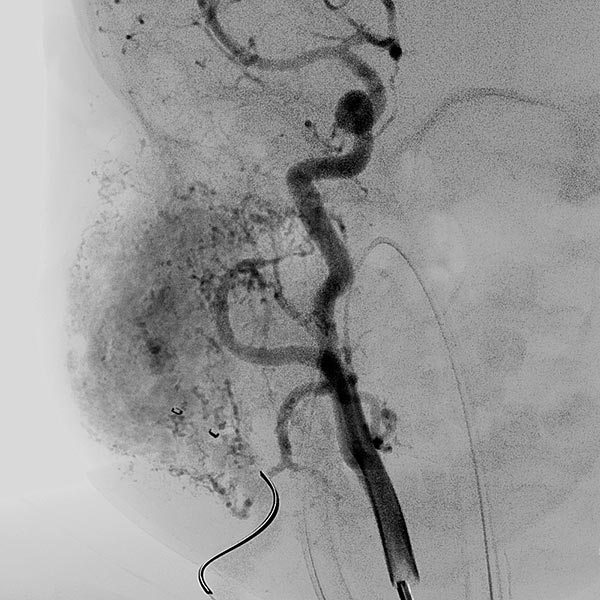
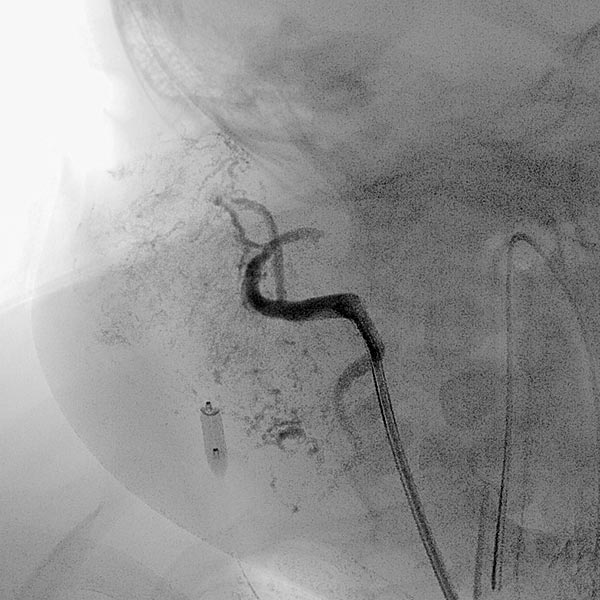
The girl is now 24 months old and the mass has not regressed. It is visible from the outside and causes the patient clear pressure pain. Dynamic contrast-enhanced MR angiography shows the intense enhancement of the infantile hemangioma. The main venous drainage is via the external jugular vein, which shows a relevant stenosis of the outflow in the proximal area.

In view of the lack of regression, probably also caused by the relevant stenosis of the venous outflow, the decision to embolize the hemangioma was made in the 24th month of life in order to induce regression of the mass. In a first step during intervention, the venous outflow (right external jugular vein) was cannulated retrogradely from transvenously.

A small balloon catheter was then inserted to block the venous outflow prior to embolization to prevent unintended dislocation of the arterially injected embolic agent to the venous side.
![Large, deep-seated infantile hemangioma [Translate to English:] Stenosis: venous outflow](/fileadmin/images/patientenbeispiele/10-ih-hals/f10-06-embolisation-infantiles-haemangiom.jpg)
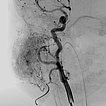
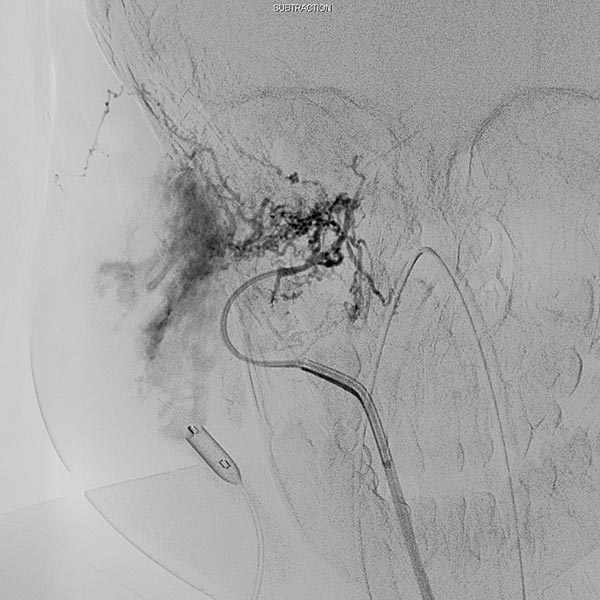
Digital subtraction angiography (DSA) after injection into the right common carotid artery shows the infantile hemangioma mainly supplied from the external carotid artery, as expected.
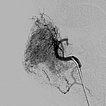
Digital subtraction angiography (DSA): After insertion of a 4F diagnostic catheter transarterially into the external carotid artery, selective advancement of a microcatheter into the maxillary artery. The infantile hemangioma presents as typical contrast pooling (“tumor blush”). The transvenously inserted balloon blocks the venous outflow and is clearly visible. Embolization was then carried out with particles of 150 micron size and without unintended venous outflow.
Control digital subtraction angiography (DSA) after first injection with particles. Part of the infantile hemangioma has already been occluded.
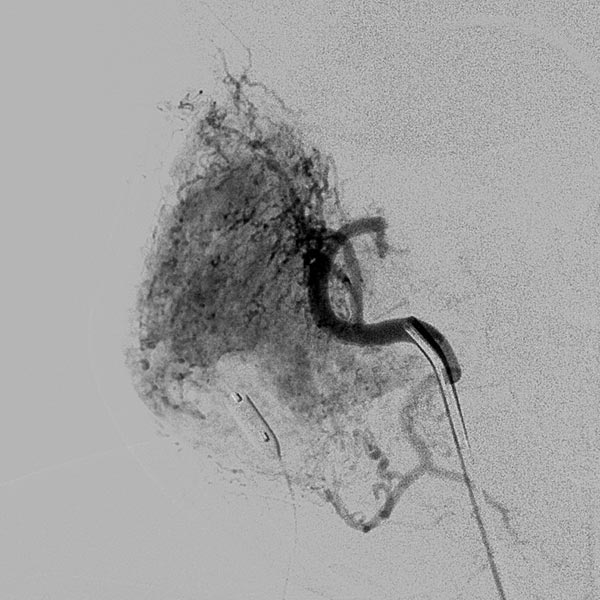
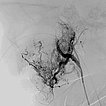
Digital subtraction angiography (DSA) after further super-selective injections with particles via a microcatheter while blocking the venous outflow. A good 50% of the infantile hemangioma has now been successfully occluded.
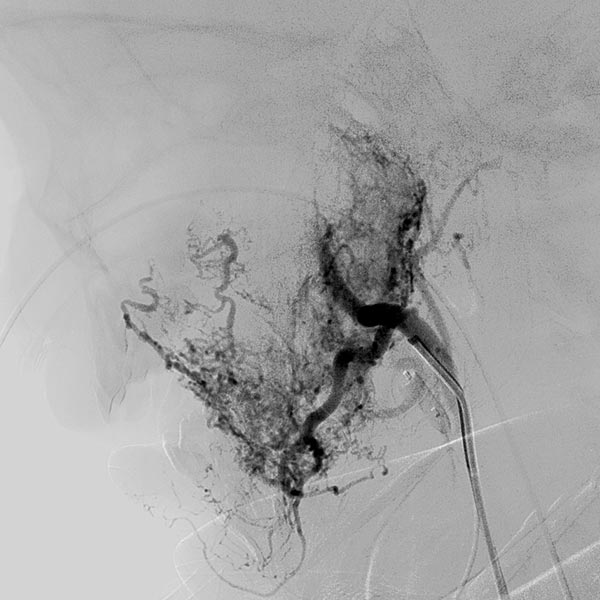
Digital subtraction angiography (DSA) after super-selective catheterization of the remaining arterial feeder supplying the infantile hemangioma.
During super-selective particle embolization (150 micron particles) via the arterial microcatheter after blocking out the venous outflow, the particles can be seen as a faintly contrasted area.
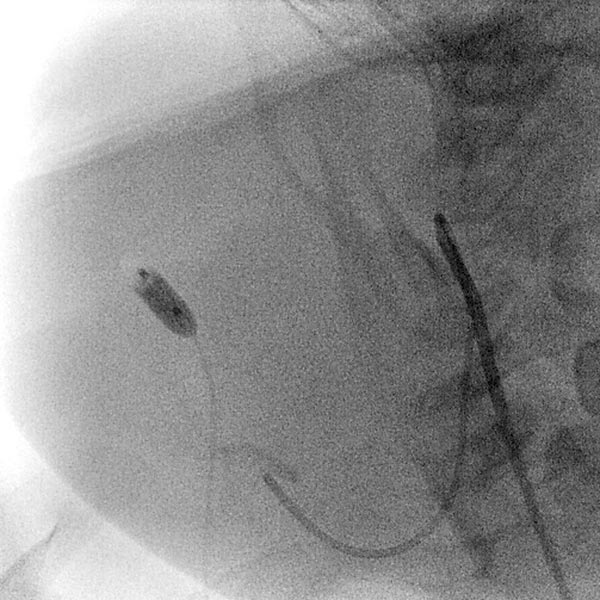
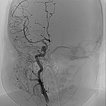
In the transarterial control angiography via the 4F diagnostic catheter, the infantile hemangioma is not perfused anymore. The typical DSA image of a “defoliated tree” is now shown.
Overview angiography via the common carotid artery after removal of the venous blocking balloon displays a virtually completely devascularized infantile hemangioma. The intracerebral circulation is normal.

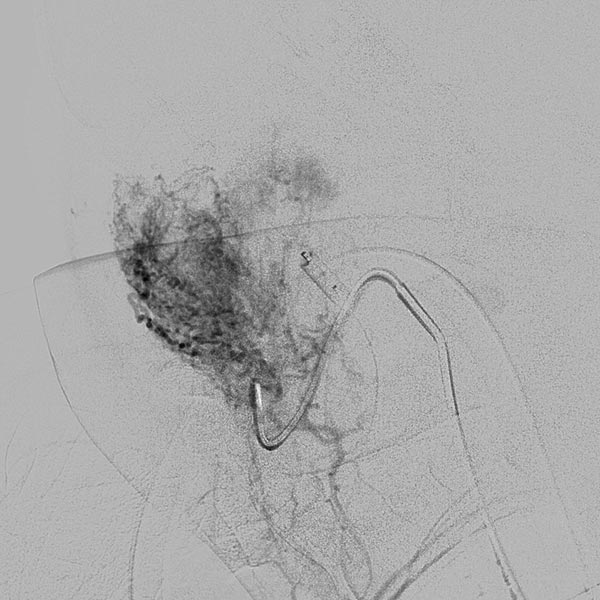
Only 6 days after embolization, the subcutaneously located infantile hemangioma has decreased substantially in volume (AP view). The overlying skin did not discolor. The patient was asymptomatic from this point on, and the infantile hemangioma completely regressed within 3 months without further therapy.

After embolization, no relevant discoloration or swelling is visible even in the lateral view.

Deeply situated infantile hemangiomas may cause local symptoms via the space-occupying effect due to their size. If medical therapy with propranolol (gold standard) alone does not show sufficient effect, invasive therapy (embolization or resection) may still be indicated in rare circumstances. The peculiarity of this case was the high-grade stenosis of the venous outflow, which probably led to insufficient regression via venous congestion. However, this stenosis could be used during embolization to simultaneously block out the venous drainage and avoid unintended dislocation of the embolic agent to the venous side. After successful embolization, infantile hemangiomas tend to regress rapidly because they are cut off from the arterial blood supply and thus from hypervascularization.
Published: 2018
All images © Wohlgemuth


![Large, deep-seated infantile hemangioma [Translate to English:] Stenosis: venous outflow](/fileadmin/_processed_/4/1/csm_f10-06-embolisation-infantiles-haemangiom_0becf48fe7.jpg)