Author(s): Wohlgemuth, Walter A.
Author(s): Wohlgemuth, Walter A.
Circumscribed, soft, slowly increasing circumscribed swelling on the right abdominal wall and flank. Two old scars after unsuccessful open partial resection. Circumscribed pain in the area of the swelling, the overlying skin is not discolored.

At the upper edge of the cranial scar, small lymphatic vesicles are visible on the skin (lymphangioma circumscriptum). At times these vesicles are secreting clear-yellowish lymph (lymphorrhea).

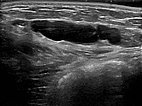
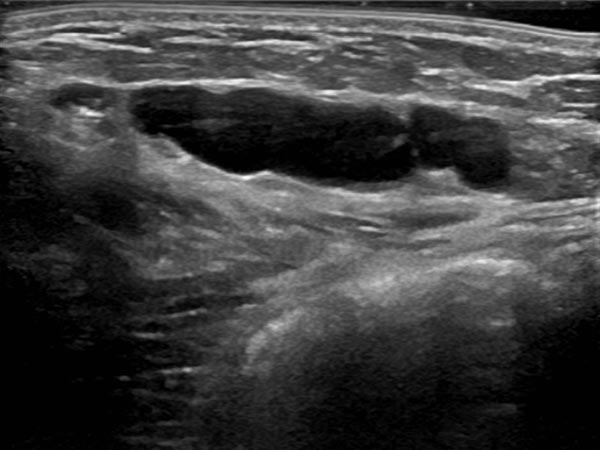
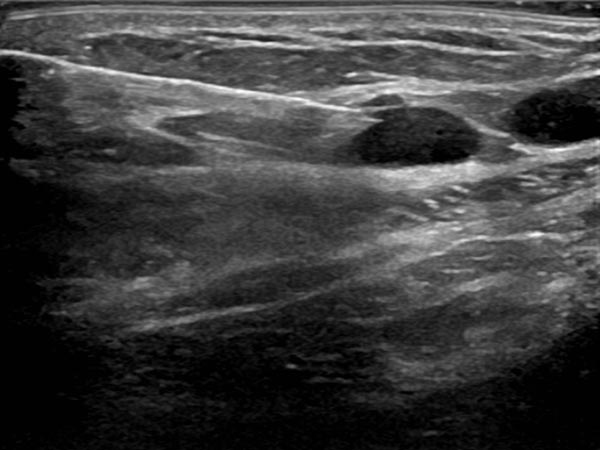
Circumscribed macrocystic malformation on the abdominal wall on ultrasound. Note the anechoic fluid in the thin-walled cystic spaces filled with liquid (lymph).
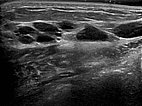
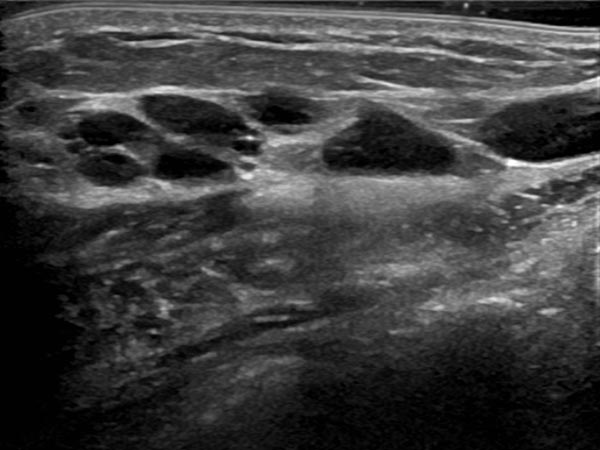
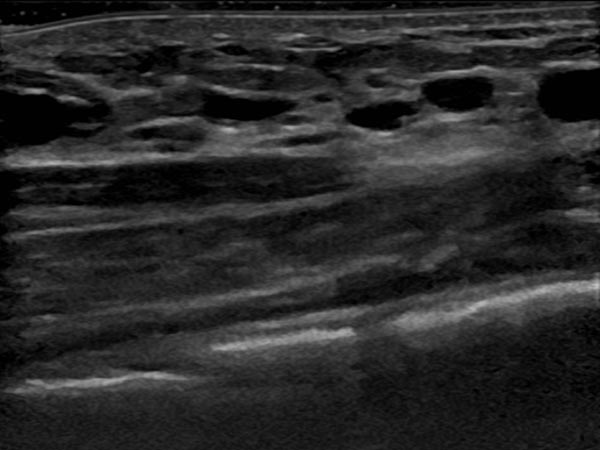
Ultrasound of the abdominal wall, a little further caudally. Here, the cystic parts of the lymphatic malformation are smaller. However, the lesion is still extraperitoneal in the abdominal wall.
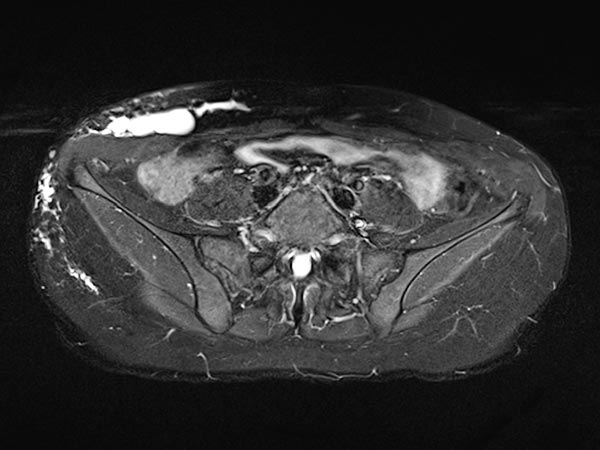
Coronal, T2-weighted, fat-suppressed MRI of the lower abdomen at the level of the groin. Normal inguinal lymph nodes. The lymphatic malformation of the abdominal wall presents as large, dysplastic, balloon-like, septated cysts that are grossly hyperintense (white).

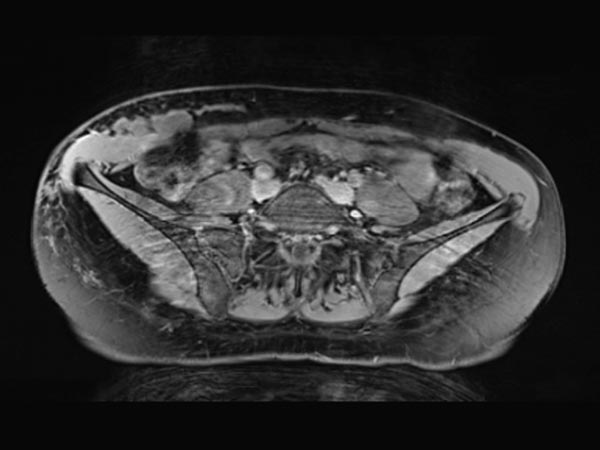
Same slice in non-enhanced T1-weighted MRI. The cysts of the lymphatic malformation are isointense to the surrounding musculature. Thus, the cysts do not contain blood or high protein content.

Transverse, T2-weighted, fat-suppressed MRI at the level of the iliac crest shows additional extension of the lymphatic malformation to the right flank. Only the epifascial portions of the abdominal wall and trunk wall are involved.
Transverse T1-weighted, fat-suppressed MRI after contrast administration shows only minimal enhancement of the thin walls of the lymphatic malformation. This is typical of a lymphatic malformation, as the liquid in the cysts (lymph) does not enhance.
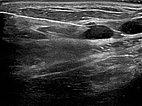
Ultrasound-guided puncture of the cystic portion of the LM during sclerotherapy. Via this puncture needle, the lymphatic malformation is first injected with contrast, then aspirated and the sclerosing agent is introduced.
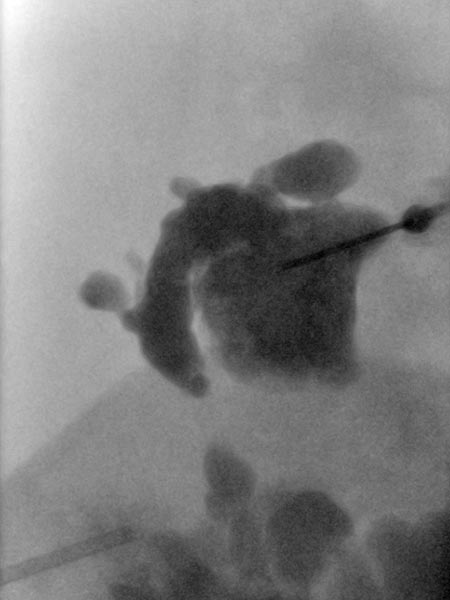
Overview X-ray in the area of the right pelvic crest after injection of contrast medium via the needle directly located in the lymphatic malformation. Large parts of the lymphatic malformation are contrasted from this needle position, representing an optimal needle position for sclerotherapy.

Additional puncture approximately 5 cm cranially into another cystic compartment of the lymphatic malformation. This compartment does not communicate with the lower part of the malformation still visible caudally. Therefore, it must be sclerosed separately in order to successfully occlude the entire lymphatic malformation.
New sclerotherapy in a second session using direct puncture technique under ultrasound guidance into the remaining cystic areas of the lymphatic malformation (X-ray overview image after contrast injection via the needle). After injection of the contrast medium, the punctured area is then evacuated of fluid as completely as possible. Then the sclerosing agent, here picibanil (OK-432), is injected via the same needle position.

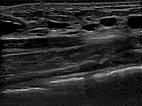
In the ultrasound examination 6 months after the 2nd sclerotherapy, only very small cystic parts of the lymphatic malformation are detectable. The larger cysts are occluded. As the patient is asymptomatic, there is no further treatment of these residual parts in an intrinsically benign lesion.
The swelling of the abdominal wall caused by the lymphatic malformation has subsided. The patient no longer has any pain. The lymphangioma circumscriptum is sealed and has completely regressed.

Macrocystic lymphatic malformations (LM) located directly on the skin can lead to lymphatic fluid oozing out via small skin vesicles (lymphatic vesicles) due to the underlying high local lymphatic pressure. These areas are called “lymphangioma circumscriptum”. Sclerotherapy (here with the agent picibanil = OK-432) closes the lymphatic channels via a strong local inflammation and seals the skin. A favorable aspect in this case were the large parts of the lymphatic malformation communicating with each other (visible after injection of contrast agent via the puncture needle). Therefore, only a few punctures were necessary to sclerose the entire lymphatic malformation. This minimally invasive procedure is usually gentler in the long run than open surgical measures. Individual smaller cysts in the often irregularly shaped lymphatic malformation can be easily reached with the liquid sclerosant.
Published: 2018
All images © Wohlgemuth