Author(s): Wohlgemuth, Walter A.
Author(s): Wohlgemuth, Walter A.
Photograph of the extension of the lymphatic malformation (LM) at 2 years of age.

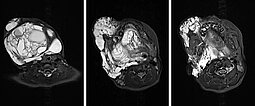
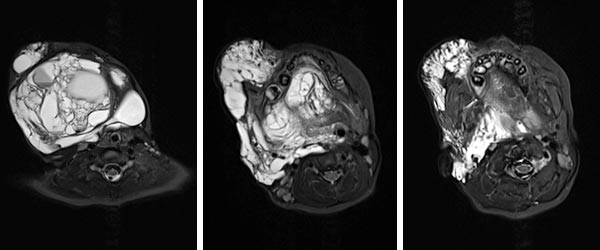
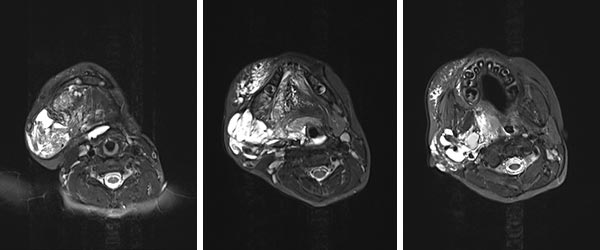
MRI (axial; T2-weighted; fat-suppressed) at 2 years of age shows the lymphatic malformation as a severely hyperintense (white) mass. The extension reaches into the deep soft tissues of the neck. Oropharynx and hypopharynx are clearly constricted. In this situation, there is a threat of upper airway obstruction if the swelling increases. This can be fatal.
The anesthesiologist succeeds in intubating the child safely and securely with fiberoptic assistance.

A pigtail catheter with many side holes is inserted for sclerotherapy of the lymphatic malformation. During aspiration, clear, yellow lymph can be aspirated from the lymphatic malformation.

Lateral view under fluoroscopy after contrast injection into a lymph cyst in the neck. Note the extension to behind the spine. The upper airway is narrowed and displaced here.

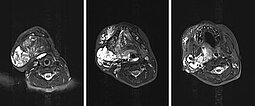
Axial T2-weighted, fat-saturated MRI at 6 years of age, after a total of 4 sclerotherapy procedures, shows a clear improvement, especially of the macrocystic parts of the lymphatic malformation. The positive effect on the upper airways, which are now no longer constricted, is also striking.
The sclerotherapy-only series was then terminated at 6 years of age (photograph). The tissue overgrowth now remaining consists mainly of adipose tissue. Lymphatic malformation components of a relevant nature are no longer found. This excess tissue can now be resected, together with the excess skin.

Lymphatic malformations (LM) in particular, but also venous malformations, can lead to considerable narrowing of the airways in the oropharynx and hypopharynx, and more rarely in the larynx as well. Additional constriction can occur if there is added swelling due to hemorrhage and bacterial inflammation in the case of lymphatic malformations, or thrombophlebitis in the case of venous malformations. However, treatment by sclerotherapy or open surgery also threatens to cause additional swelling. This must be anticipated and, if necessary, the patient must be intubated until the postoperative swelling subsides. Prior information to the anesthesiologist is essential so that he or she can prepare for a potentially difficult intubation. Prior endoscopic examination of the upper airway by ENT colleagues is often very helpful in this case.
However, consistent therapy, with close interdisciplinary coordination, can even resolve this difficult situation.
Published: 2020
All images © Wohlgemuth