Author(s): Sadick, Maliha
Author(s): Sadick, Maliha
26-year-old female patient with recurrence of AVM at digit III of the right hand. Dorsal and palmar view after transarterial embolization 2 years ago. Recurrent, painful swelling of D III with palpable pulsations and a thrill.

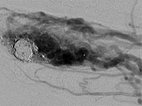
After incomplete transarterial embolization of the AVM 2 years ago, a recurrence of the AVM has appeared. During previous embolization only a part of the AVM was occluded, which actually increases the risk of recurrence. The old radiopaque embolic agent of the previous embolization can be seen centrally in the nidus.
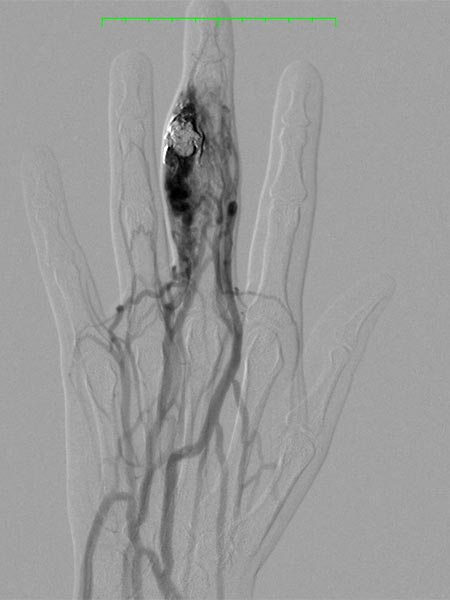
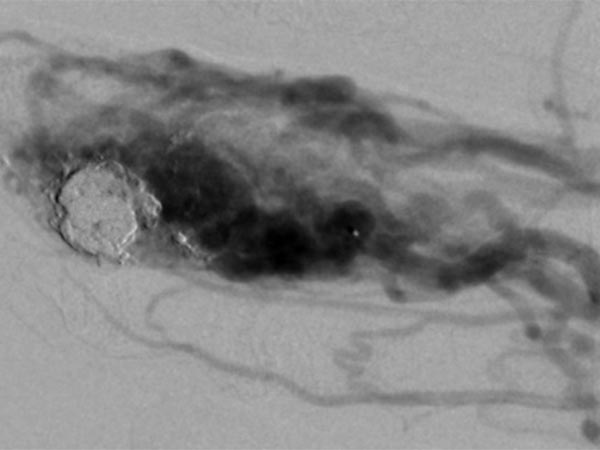
The nidus of the AVM in a magnified target image of the D III in digital subtraction angiography shows significant increase in size compared to the old angiographies (not shown). DSA images after transarterial antegrade puncture of the brachial artery with hypervascularized AVM of the middle and distal phalanx.
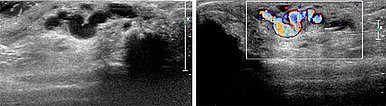
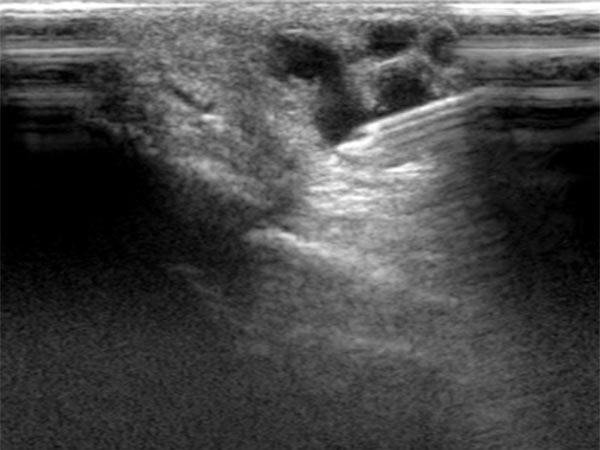
Ultrasound reveals a subcutaneous dilated drainage vein from the digital AVM at the third finger. Color-coded duplex ultrasound (CCDU) confirms the fast-flow arteriovenous shunt with high flow.
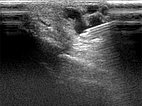
Since it seems technically impossible to treat the AVM via a transarterial approach alone for re-embolization, a percutaneous access route in the direct puncture technique is now selected under sonographic guidance.
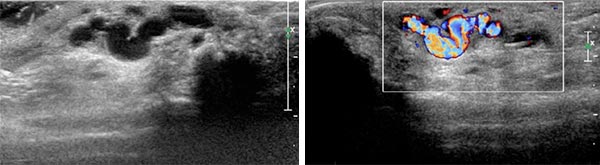
Percutaneous ultrasound-guided advancement of the puncture needle into the drainage vein of the digital AVM.
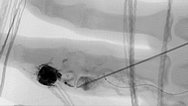
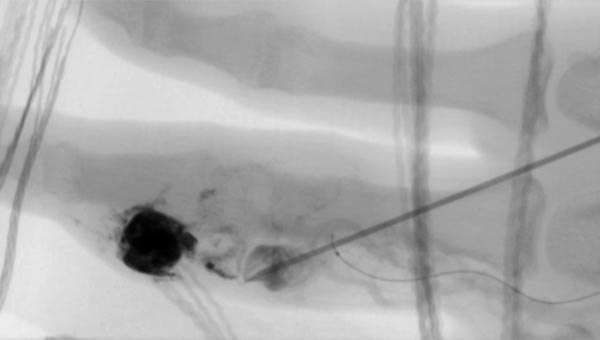
Fluoroscopic view of the puncture needle at the start of direct percutaneous embolization therapy of the finger with a liquid embolic agent (EVOH). The microcatheter which has been advanced to the nidus is additionally visible.
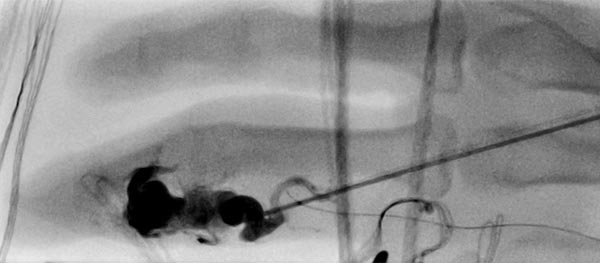
Fluoroscopic control after successful nidus embolization of the AVM. The transarterially inserted microcatheter was left in place during percutaneous embolization as a landmark for the feeding digitalis propria artery. In addition, radiopaque markers are displayed by gauze placed on the skin.
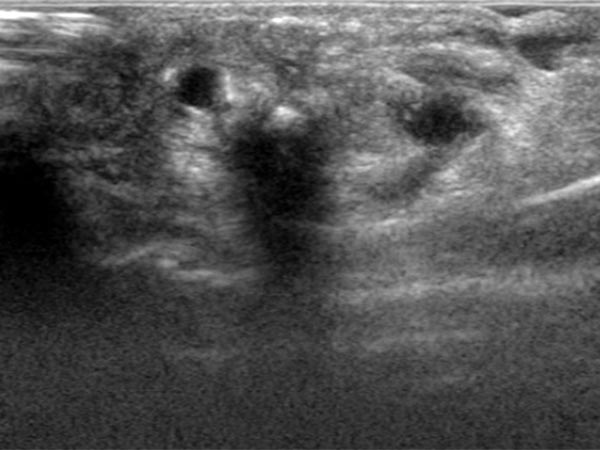
After embolization now clearly echogenic formations in the embolized vessel with dorsal acoustic shadowing due to the embolic agent after filling of the AVM nidus.
Angiographic control of the right hand with catheter injection from transarterially via the ulnar artery. Complete devascularization of the AVM nidus. No fast-flow shunts can be angiographically detected. The treated AVM with occluded nidus is thus resectable.

Fluoroscopic view of the cast after successful nidus embolization of the AVM. To improve the overview for surgical planning, this image is also shown without subtraction with visible bone.

Palmar and dorsal view of D III right hand 5 days after percutaneous embolization. Marked swelling after embolization along the third finger on the ulnar side. Clinically, pain and pulsations or a thrill in the finger are now gone with intact sensory and motor function.

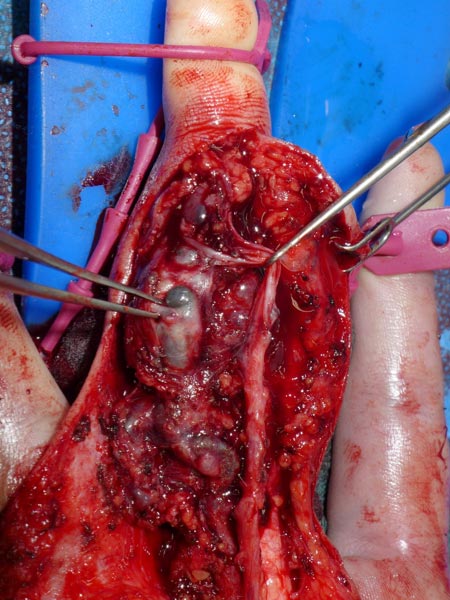
Intraoperative photograph during microsurgical dissection of the middle finger on the right for removal of the embolized nidus. The black embolic agent is visible centrally in the embolized vessels.
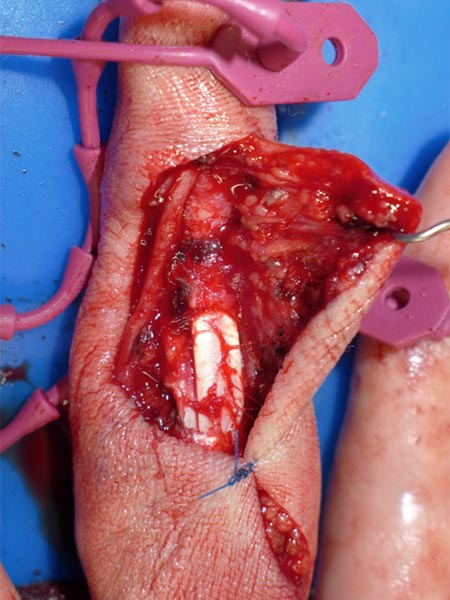
Intraoperative image after complete resection of the embolized nidus before final suturing of the surgical wound.
The recurrence of an arteriovenous malformation (AVM) of the right D III finger demonstrated in this case after previous incomplete embolization was re-embolized via a direct percutaneous access. This was done to allow the subsequent resection to be as radical as possible to avoid further recurrence. Ultrasound and fluoroscopy were very valuable methods for planning and performing the procedure.
After successful occlusion of the nidus under sonographic and angiographic guidance, surgical resection of the occluded nidus was subsequently performed.
Transarterial access to an AVM is very relevant for intraprocedural imaging and control but is not necessarily the sole treatment access.
In the case of complex anatomic conditions with very difficult access via a transarterial microcatheter, percutaneous embolization of the AVM using a direct puncture technique should be considered, especially in AVMs with dilated drainage veins. Ultrasound with color duplex is a valuable diagnostic tool for this purpose.
Published: 2018
All images © Sadick