Author(s): Wohlgemuth, Walter A.
Author(s): Wohlgemuth, Walter A.
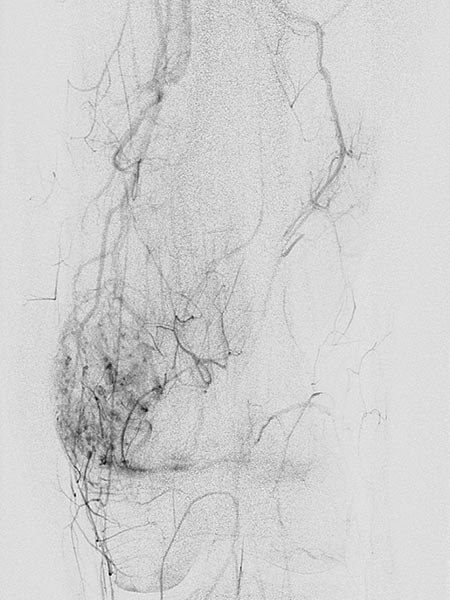
13-year-old female patient with recurrent painful swelling at the medial distal left thigh. Condition after surgical exploration, which was aborted due to severe bleeding. Histologically a "hemangioma" was diagnosed. However, this diagnosis does not correspond to the biological behavior of the lesion. Postoperatively no improvement of the exercise-dependent pain.

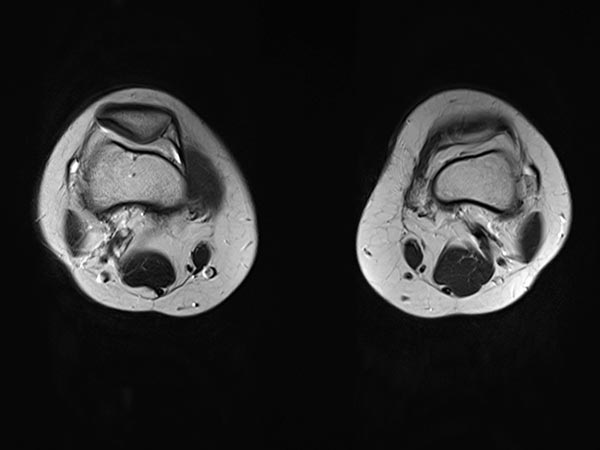
Axial T2-weighted MRI shows a hyperintense, homogeneous mass in the area of the swelling. Morphology very compatible with a venous malformation. Strikingly, some smaller central flow voids suggestive of arteries in the lesion.
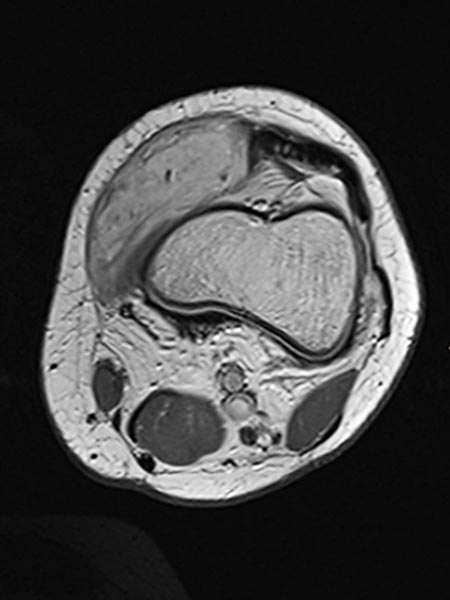
The axial T2-weighted, fat-saturated MRI slightly more cranial again depicts typical signs of a venous malformation with severe hyperintensity of the lesion.
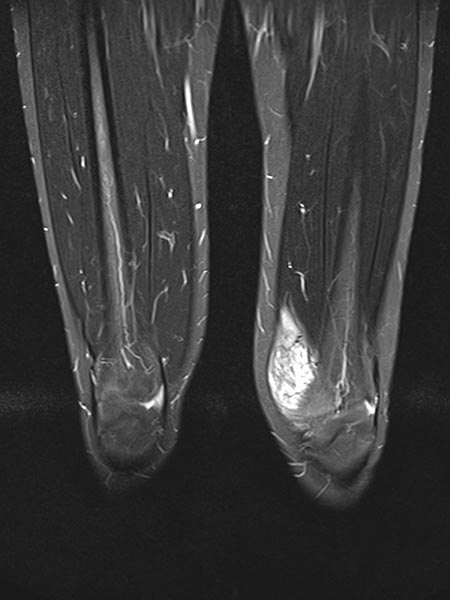
In coronal T2-weighted, fat-suppressed MRI, the extent of the strongly hyperintense venous malformation in the cranio-caudal direction is delineated.
Dynamic contrast-enhanced MR angiography in an early, arterial phase shows early enhancement with arterial vascularization of the venous malformation. This indicates arteriovenous fistulas in the venous malformation.

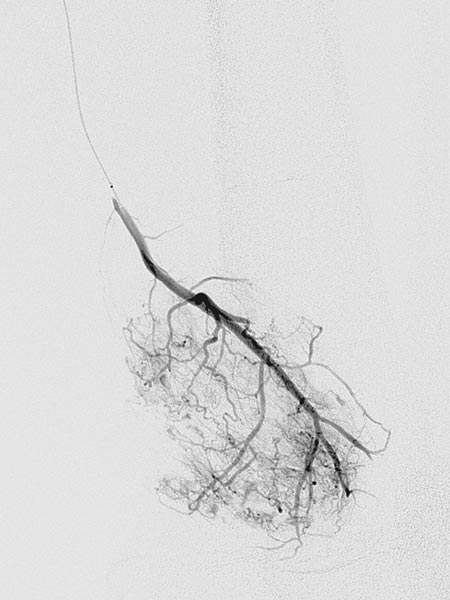
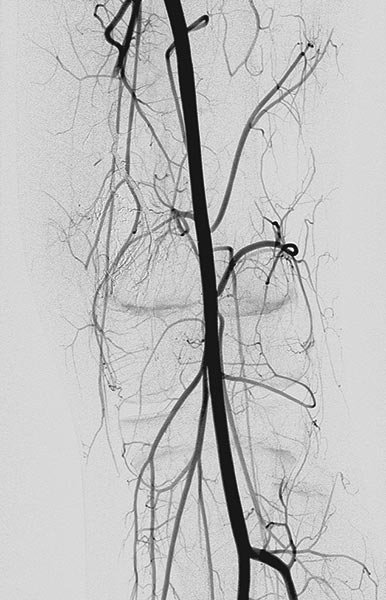
Digital subtraction angiography (DSA) in the early arterial phase shows a dilated feeding artery (so-called “feeder artery”), in this case a medial superior genicular artery. This artery is dilated over time due to chronic hyperperfusion with increased blood flow.

Digital subtraction angiography (DSA) in the arterial phase 2 s later shows some minor arteriovenous fistulas.

Digital subtraction angiography (DSA) in the interstitial and early venous phase again 4 s later shows no direct early venous outflow of the contrast agent but, instead, a pooling phenomenon. In an arteriovenous malformation, an immediate venous outflow would be seen because of multiple direct arteriovenous communications.
Super-selective catheterization of the feeding artery with a microcatheter again depicts multiple, fine arteriovenous fistulas, but not the immediate venous outflow as would be typical of an AVM. However, the visible arteriovenous fistulas are unusually prominent in this venous malformation.
The microcatheter is now used to selectively embolize the fistulas with ethylene-vinyl alcohol copolymer, which as a liquid agent is distributed throughout the fine fistulae.
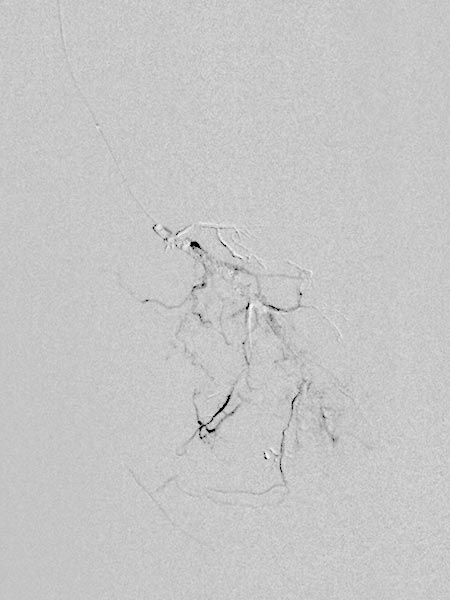
The radiographic overview after embolization of the AV fistulas shows the selective cast specimen of the radiopaque embolic agent filling the fistulas.
In the final overview digital subtraction angiography after embolization, the fistulas are completely occluded.
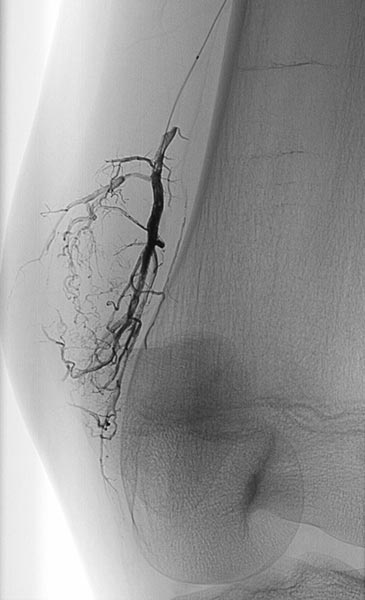
In the same session, sclerotherapy is performed using the direct puncture technique. Under ultrasound guidance, the venous malformation is punctured and contrast medium is injected.

A draining vein was immediately contrasted, which drains into the femoral vein and thus communicates with the deep conducting venous system. This communication was occluded with ethanol gel.

After occlusion of the drainage, complete sclerotherapy of the VM was possible because the liquid sclerosing agent could no longer drain off via the communicating vein.

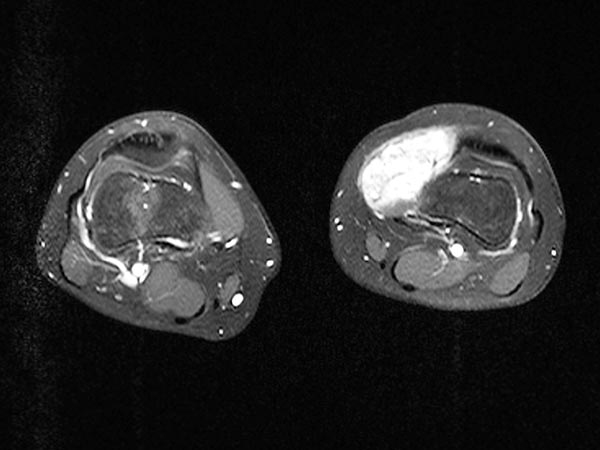
The completely occluded venous malformation, which in this case had contained multiple arteriovenous fistulas, was successfully resected after successful embolization and sclerotherapy with complete occlusion. Axial T2-weighted MRI demonstrates the completeness of the resection without a remaining lesion.
The completely occluded venous malformation was successfully resected after successful embolization and sclerotherapy following complete occlusion. The patient has thus far been asymptomatic (3 years, 4 months).

The venous malformation (VM) presented with severe intraoperative bleeding during an initial incomplete open resection attempt. On further evaluation, MR angiography revealed multiple atypical arteriovenous fistulas in the venous malformation, but not the typical behavior of an AVM with immediate venous outflow.
The venous malformation was therefore completely embolized from a transarterial access, which is normally not necessary in a venous malformation.
As an added complication, a clear communication with the deep conducting venous system of the leg was found, which had to be occluded before sclerotherapy, in this case with ethanol gel. Subsequently, complete sclerotherapy was performed.
The occluded venous malformation was then completely resected without complications or increased bleeding. The venous malformation has remained asymptomatic to date, and recurrence is not expected.
Published: 2018
All images © Wohlgemuth