Author(s): Wohlgemuth, Walter A.
Author(s): Wohlgemuth, Walter A.
13-year-old female patient with chronic pain and progressive hard palpable swelling and volume increase of the left calf over a period of more than 4 years (posterior view). During the past 1.5 years, a progressive pes equinus has additionally occurred on the left side. The overlying skin is minimally bluish discolored. The right leg is longer than the left. The combination of chronic, continuous pain and progressive pes equinus suggests a special form of venous malformation, known as a Fibro-Adipose Vascular Anomaly (FAVA). In addition to venous malformation and fatty tissue, this lesion consists of connective tissue, which increasingly contracts.

In the lateral view, the local volume increase is more conspicuous.

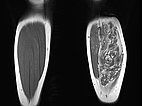
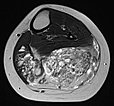
Coronal T1-weighted non-enhanced MRI shows an intramuscular, vascular lesion (isointense to the muscle) with marked interstitial hyperintense adipose tissue. This fatty tissue is more pronounced than would be usual in a normal venous malformation.
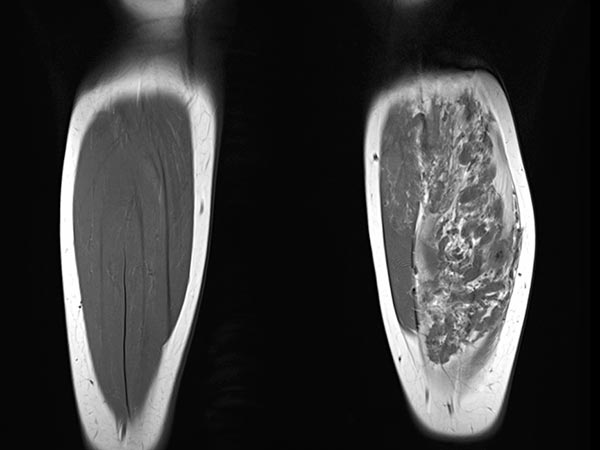
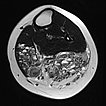
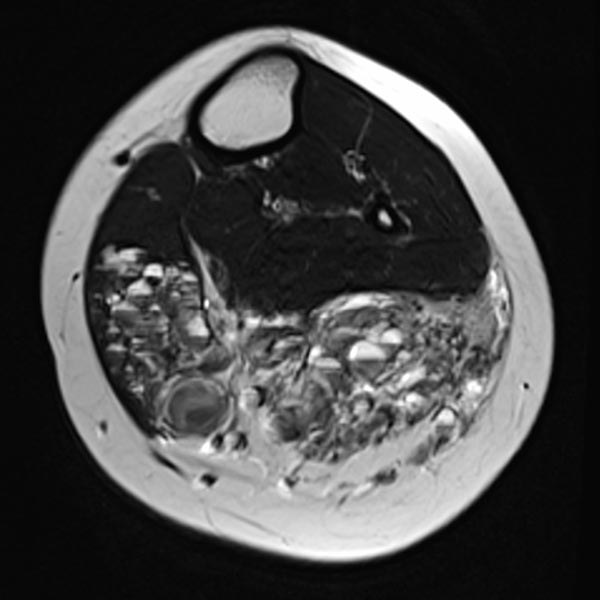
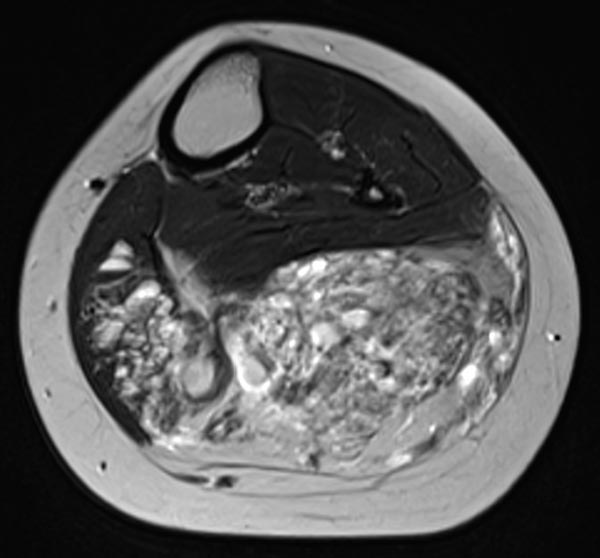
Axial T2-weighted MRI of the left lower leg shows multiple dilated, dysplastic veins in a venous malformation throughout the superficial flexor muscles. Slow flow causes stasis of the blood within the malformation with the formation of fluid-fluid levels. Almost the entire muscle consists of malformation and fatty tissue. Also visible is a large thrombus in a dilated, dysplastic vein.
Contrast-enhanced MR angiography (MIP) shows complete enhancement of the venous malformation component in the left calf with contrast pooling.

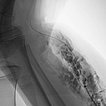
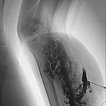
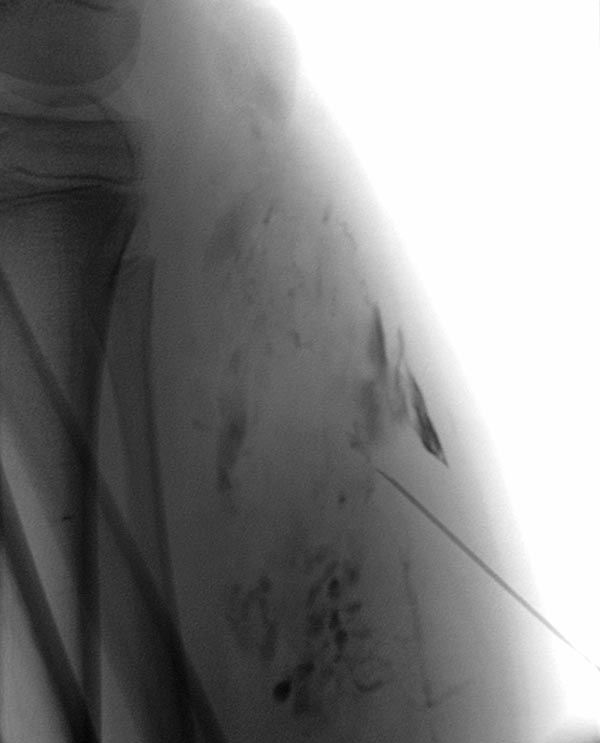
Phlebography after direct puncture of the venous malformation shows a large-lumen drainage vein communicating with the popliteal vein in the popliteal fossa. This must be occluded before sclerotherapy, otherwise the sclerosing agent could unintentionally dislocate through this communication and potentially cause thrombosis of the deep venous system of the leg and/or pulmonary embolism. In addition, there is an ongoing, increased risk of thromboembolism in this patient even outside of sclerotherapy, which can be significantly reduced by occlusion of the communication.
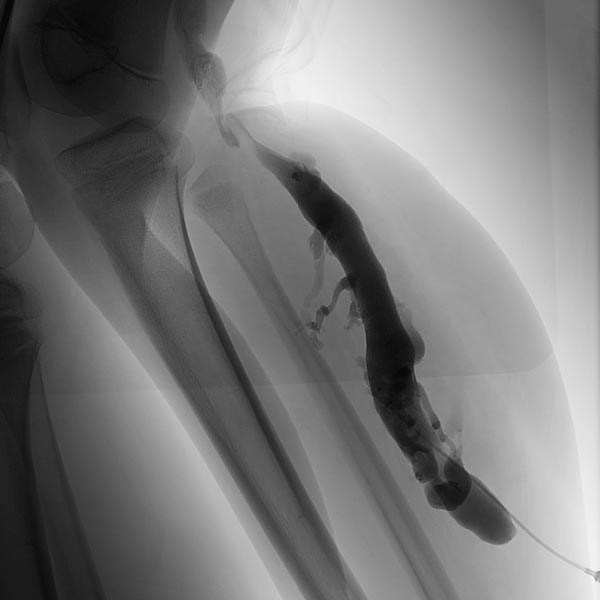
To occlude the vein, a large-lumen introducer sheath is first advanced via a guidewire. This sheath is used to insert the laser fiber and is advanced via the vein to the communication point in the popliteal fossa.
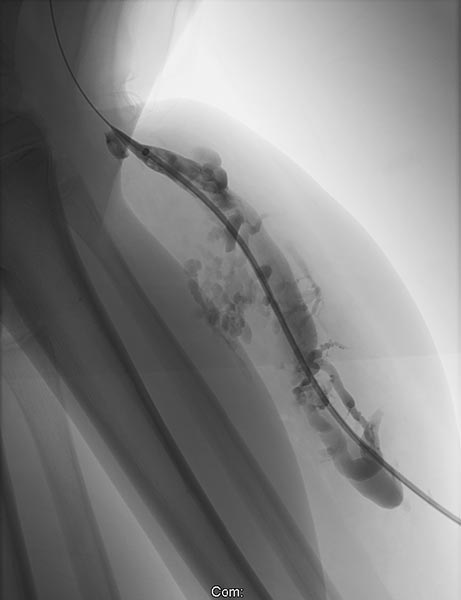
A laser fiber is advanced through this sheath for endovascular laser therapy. The heat of the laser beam causes massive irritation of the vein wall, which subsequently closes quickly. Thrombus formation immediately occurs around the laser tip.

After occlusion via laser fiber and contrast injection via the pulled-back introducer sheath, there is no more outflow of the contrast medium via the communicating vein. Thus the communication is successfully occluded. Only the venous malformation is still contrasted. This is now ready for sclerotherapy, as the sclerosing agent can no longer drain into the deep venous system of the leg.

After additional puncture of a very distal part of the large-lumen communicating vein and contrast injection, there is no more outflow into the deep venous system. Thus, even in the long term, the risk of embolism of thrombi from the venous malformation into central conducting veins is eliminated.
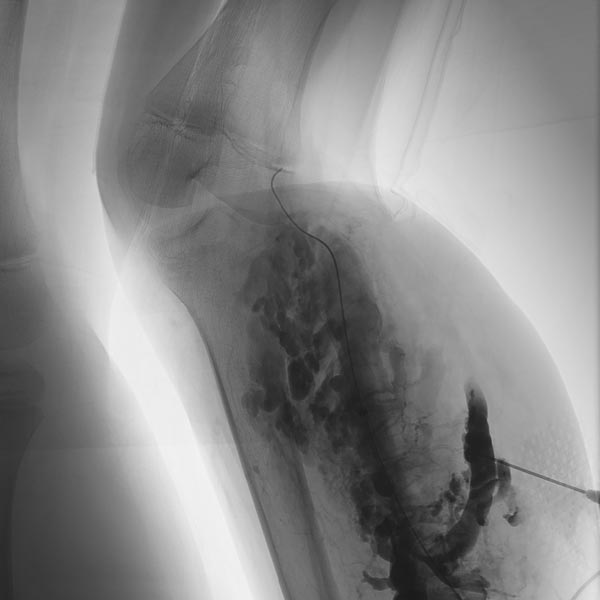
Additional sclerotherapy 3 months after the first treatment with polidocanol foam 3% with ultrasound-guided direct puncture. The more proximal parts of the venous malformation are partially occluded, the still open channels of the venous malformation after the first treatment are significantly reduced in size. The former communication with the deep conducting venous system remains occluded. In the meantime, a temporary epiphysiodesis with temporary stapling of the growth plates had been performed for leg length correction on the other side.

A new puncture was performed more proximally on the lower leg because still open parts of the venous malformation were detectable here on ultrasound. After contrast injection, only a few, small-lumen areas of the venous malformation are contrasted. Sclerosing foam can be seen in the cavities of the distal part of the venous malformation (visible as intraluminal radiolucency).
The control MR angiography shows a clear improvement of the findings. Most of the dysplastic, dilated channels of the venous malformation are occluded.

In coronal, non-enhanced T1-weighted control MRI, the vascular component of the lesion is less conspicuous. However, clearly additional soft tissue remains that is pathologic (“salt-and-pepper pattern”). This tissue consists in part of hyperintense adipose tissue and in part of hypointense connective tissue. This is the typical MRI appearance of a fibro-adipose vascular anomaly (FAVA).
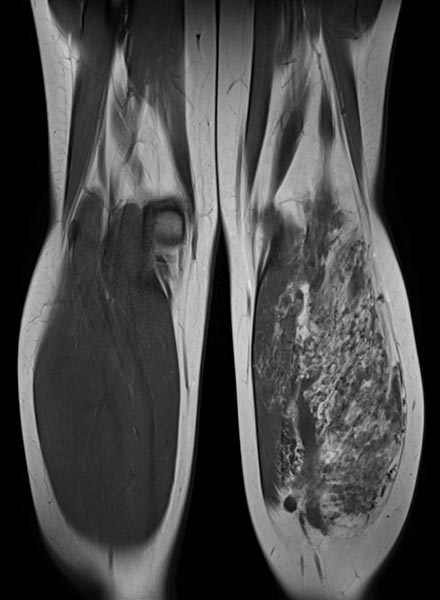
The vascular channels are largely occluded on axial control MRI in T2-weighted images. However, after successful occlusion of the vascular channels, a black-and-white “salt-and-pepper” pattern typical of FAVA remains. This consists of adipose tissue (hyperintense) and connective tissue (hypointense).
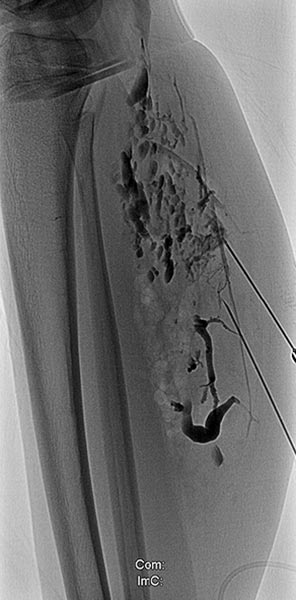
The last remaining open vascular channels of the venous malformation are now further treated with ethanol gel in an additional sclerotherapy session. The image shows a phlebography using the direct puncture technique. Ethanol gel as the sclerosing agent is particularly effective and, due to its high viscosity, less in danger of leaking into the deep conducting venous system via remaining connections or draining veins.

Injection of the ethanol gel (not radiopaque) results in displacement of the contrast agent by the gel.
After this treatment, the patient's pain improved significantly. She rarely suffered from left calf pain thereafter, mainly after heavier physical exertion. In the meantime, successful open surgical Achilles tendon lengthening had been performed to eliminate the pes equinus. This could be performed without the risk of increased bleeding due to the previous occlusion of the venous malformation.
Clinical control of the fully grown patient, now aged 17 (image taken from behind). The symptomatology has almost completely regressed. The volume and skin color of the affected left calf is now better aligned with the right side. A clinically relevant leg length discrepancy no longer exists after successful temporary epiphysiodesis of the right leg. After full body height is attained, the probability of recurrence is significantly lower with FAVA.

Clinical control of the adult patient, now aged 17 (lateral view).

Fibro-Adipose Vascular Anomaly (FAVA) is a rare subtype of venous malformation. It is always located intramuscularly (usually in the calf) and consists of additional fatty tissue and increased connective tissue besides the venous malformation. Patients suffer from a continuous pain that is particularly difficult to treat. FAVA leads to a slowly progressive muscle contracture caused by the slowly contracting abundant connective tissue (similar to a scar), in this case with a pes equinus.
In the presented patient, an additional difficulty was a large communicating vein draining into the deep conducting venous system of the leg. This communication was closed before sclerotherapy by means of endovascular laser therapy. Multiple sclerotherapy sessions thereafter resulted in significant improvement with only minor pain after a total of 2 years of treatment. The Achilles tendon was surgically lengthened to treat the pronounced pes equinus. A temporary epiphysiodesis for leg length adjustment was also successful.
Published: 2018
All images © Wohlgemuth