Author(s): Wohlgemuth, Walter A.
Author(s): Wohlgemuth, Walter A.
6-month-old girl with a relatively hard, hyperthermic mass on the medial corner of the left upper eyelid. The mass was not present at birth, increased slowly month by month and is now causing visual problems (bulbar deviation and impending deprivation amblyopia) by covering the pupil. Because of the predominantly subcutaneous location, the tumor is not raspberry red but rather bluish in color.

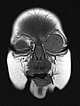
Coronal plane of T1-weighted MRI without contrast shows the mass homogeneously hypointense. Centrally, a few small flow voids visible, caused by strongly perfused arterial vessels.

T1-weighted, coronal MRI after contrast depicts a homogeneous, strong enhancement in a solid, sharply demarcated tumor of the left eye. This is suggestive of an infantile hemangioma as part of the spectrum of vascular tumors.

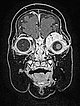
T1-weighted coronal plane MRI after contrast administration in a slightly more dorsal plane shows extension of the contrast-enhancing solid mass well into the medial orbit of the left eye with displacement of the eyeball caudally and laterally.

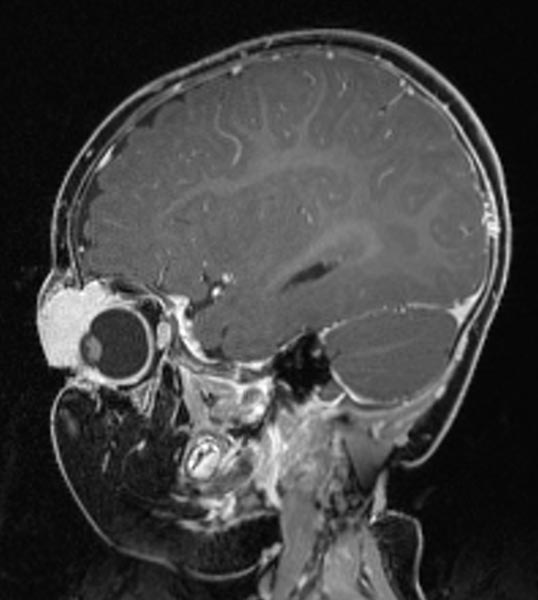
T1-weighted sagittal MRI after contrast administration. The bulb of the left eye is displaced caudally and dorsally by the expansion of the mass intraorbitally and the eyeball is depressed.
T2-weighted axial MRI with fat saturation. The mass medial to the left eye is relatively homogeneously hyperintense and sharply demarcated from the surrounding tissue. As a sign of strong arterial perfusion, some black, signal-free arterial vessels are seen in the lesion (“flow voids”). This is also typical of an infantile hemangioma.
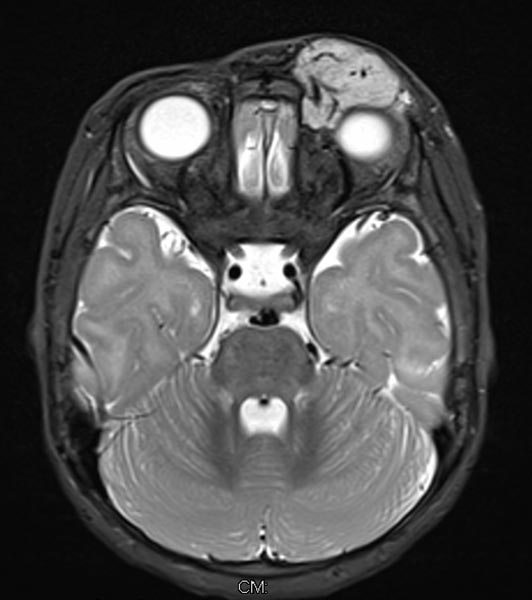
T2-weighted axial MRI without fat saturation. The mass medial to the left eye is also relatively homogeneously hyperintense in this sequence and shows central flow voids. However, due to the lack of fat saturation, the mass is not as well demarcated from the surrounding adipose tissue.

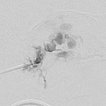
Dynamic contrast-enhanced MR angiography of the skull and cerebral vessels. In the very early arterial phase (A) no yet enhancement of the lesion in the left eye.
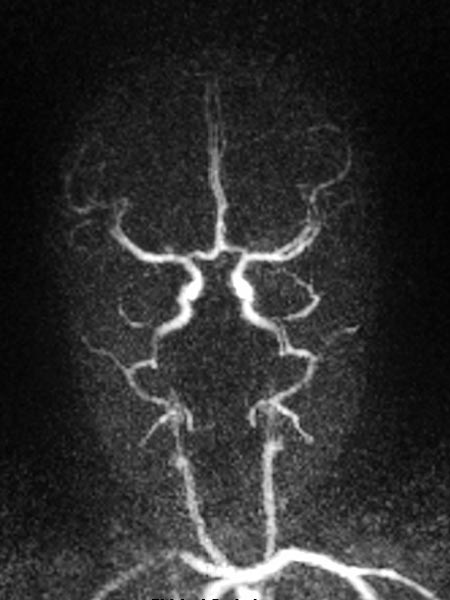
Dynamic contrast-enhanced MR-angiography in the arterial phase, 5 seconds later, depicts early and intense enhancement of the tumor in the left eye.

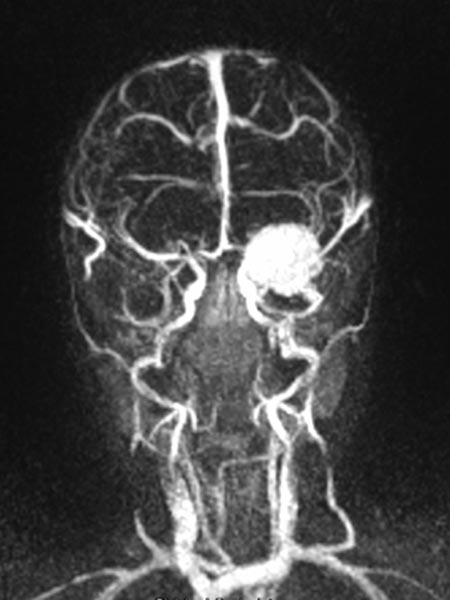
Dynamic, contrast-enhanced MR angiography, early venous phase. The strong enhancement remains, venous drainage via the facial veins and the left-sided external jugular vein.
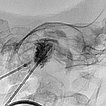
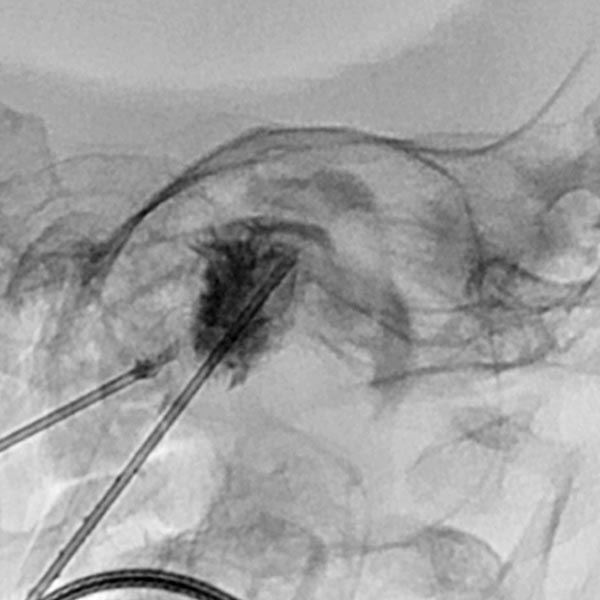
In view of the hypervascularization and the extension into the orbit, a preoperative embolization was performed with ethylene-vinyl alcohol copolymer in a direct puncture technique. Intraoperative DSA with venous drainage is depicted here.
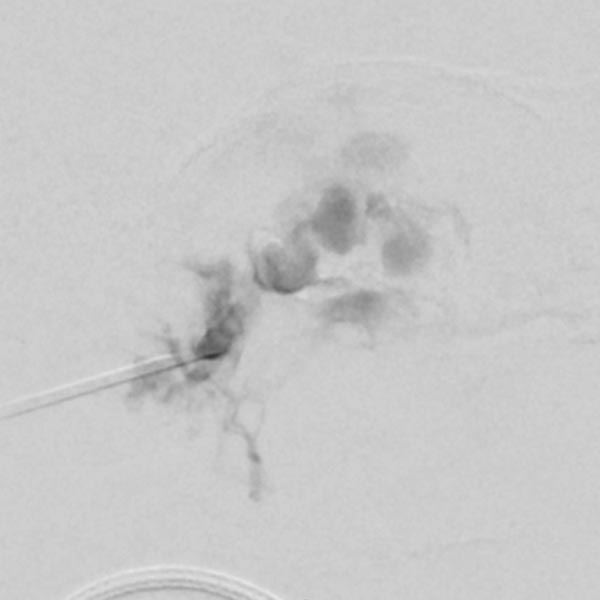
The X-ray fluoroscopy image shows the embolic agent within the vessels in black (radiopaque). The perfusion of the infantile hemangioma was super-selectively reduced.
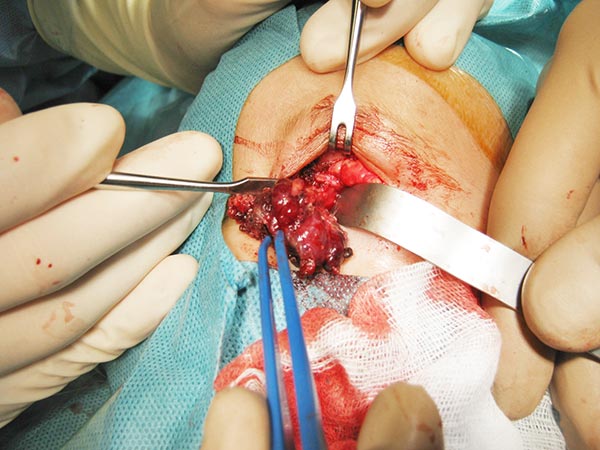
Intraoperative site (Prof. Jaegle, University Medical Center Regensburg). The dark red mass could be dissected from the orbit and the upper eyelid with relatively little blood loss while preserving the levator palpebrae muscle. The black dots in the tumor correspond to the embolic agent.
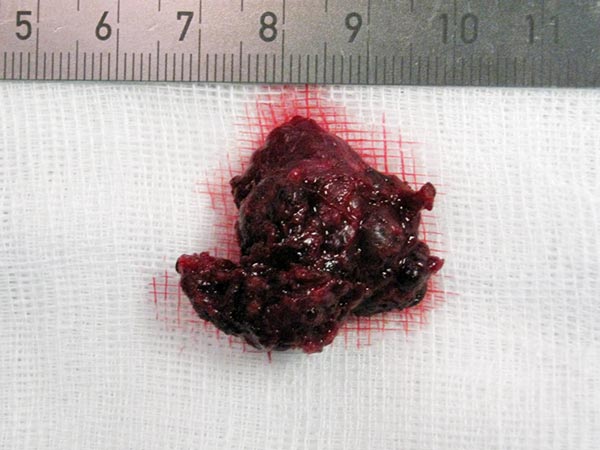
The resection specimen of the infantile hemangioma is homogeneously red due to the strong vascularization. The embolized vessels are completely filled with multiple black worm-like casts of the embolic agent, ethylene-vinyl alcohol copolymer.
Immediately postoperative image: complete removal of the mass. Inconspicuous postoperative course, the infantile hemangioma could be removed completely and without recurrence.

No recurrence at the outpatient follow-up examination 4 years and 1 month after the procedures. Three-dimensional vision is preserved, no amblyopia has developed in the left eye.

No recurrence at the outpatient follow-up 4 years and 1 month after the procedures. The upper eyelid on the left side is mobile and fully capable of closure.

Infantile hemangiomas of the eye and orbit may be a challenge even today in the era of successful drug therapy (propranolol). The rapid growth may cause pressure on the eyeball, and the lid may not be able to open. Normal development of the growing eye and visual ability or cortical visual processing may be threatened in this situation. Preoperative elimination or reduction of blood flow by embolization and microsurgical resection (combination therapy) can often achieve good results even in this difficult situation.
Published: 2018
All images © Wohlgemuth