Author(s): Wohlgemuth, Walter A.
Author(s): Wohlgemuth, Walter A.
Photograph of a girl, one year old at the time, with Klippel-Trénaunay syndrome in the form of a combined capillary-venolymphatic malformation (CVLM) with concomitant overgrowth of the affected right leg and buttock. The large, circumscribed, capillary malformation located laterally on the thigh and knee is typical.

The photograph of the same one-year-old girl with Klippel-Trénaunay syndrome (KTS) from the dorsal view shows enlargement of the right leg and buttock compared to the other side. Thus, the overgrowth involves the entire right lower quadrant of the body. Parts of the volume increase are due to accompanying lymphedema of the right leg.

At this time, the primary lymphedema still affects the right lower leg and the right heel more markedly, as is clearly visible when comparing sides. The forefoot and the toes on the right are hardly affected. It is more a circumscribed primary lymphedema typical of KTS than classic secondary stasis edema, in which the extremity enlarges from distal to proximal.

Inflammation of the cutaneous lymphatic malformation parts with recurrent erysipelas occurs again and again. In this context, there is often a recurrent increase in volume of the blood-tinged lymphorrhea from the petechiae on the large capillary malformation laterally on the knee and thigh (here covered with compresses).

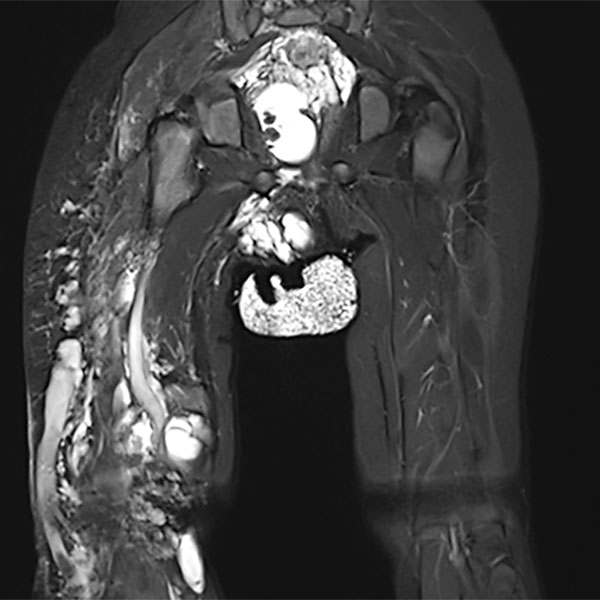
Coronal T2-weighted, fat-suppressed MRI of the pelvis and thighs shows the large extension of the malformation. Multiple sections with microcystic and macrocystic lymphatic malformation components. In addition, an extensive venous malformation with a large marginal vein laterally on the right thigh.
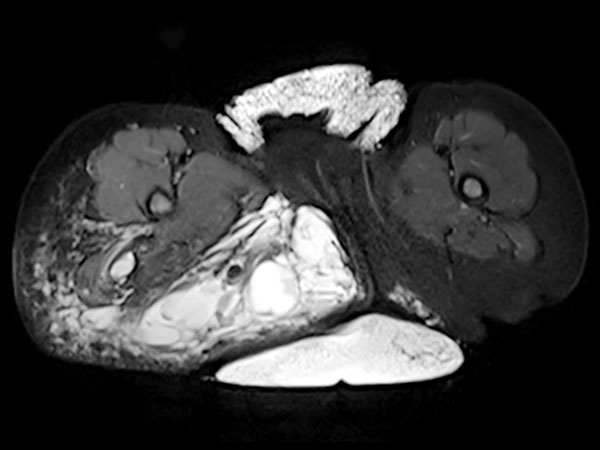
The corresponding axial, T2-weighted, fat-suppressed MRI of the pelvis at the level of the buttocks shows the massive extension especially of the lymphatic malformation in the right gluteal area. Additionally, persistent embryonic sciatic vein in the sense of a venous malformation is depicted.
Intraoperative photograph during sclerotherapy. Multiple needles are used to puncture the lymphatic malformation, which lies directly underneath the capillary malformation and is responsible for the frequent leakage of blood-stained lymphatic fluid (lymphorrhea) from the multiple small petechial clustered vesicles.. After visualization by contrast injection to ensure correct needle location in the lymphatic malformation, sclerosant is administered through the needle.

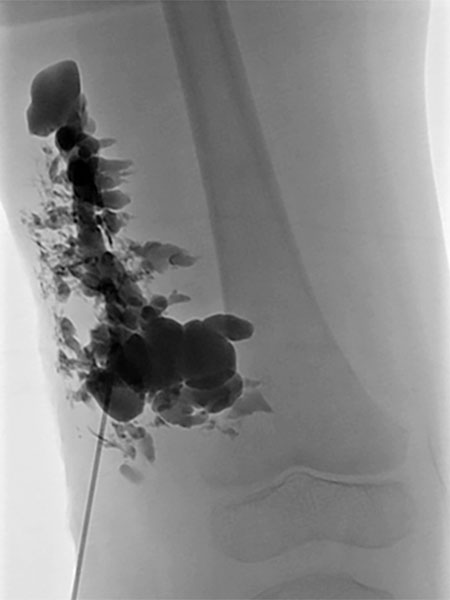
Lymphography with contrast injection directly into the lymphatic malformation subcutaneously, underneath the capillary malformation laterally on the thigh which is visible on the skin. The entire lymphatic malformation is contrasted from this needle position. Thus the ideal position for sclerosing this portion.
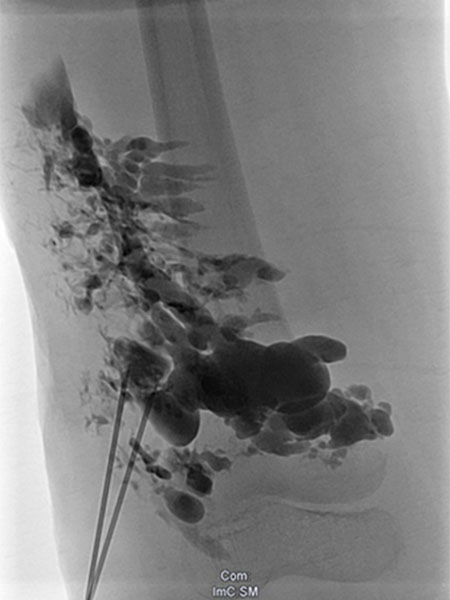
Re-puncture and lymphography with contrast injection will contrast additional parts of the lymphatic malformation, which can then be sclerosed.
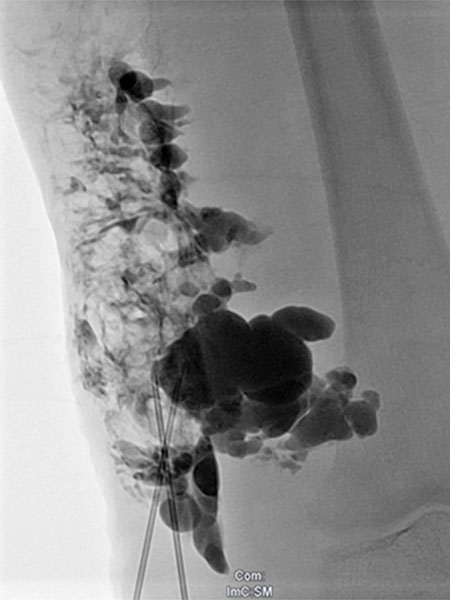
Injection of sclerosant (in this case picibanil = OK-432), which is in itself non-contrasting, displaces the previously injected contrast. In this way, the entire lymphatic malformation is sclerosed in successive steps. This results in sealing of the skin and decreases future lymphorrhea. The marginal vein is additionally occluded by radiofrequency ablation (not shown) to prevent thromboembolism.
The further course of the girl's disease was very good. In the photograph, she is 4¾ years old. She is fully mobile and only rarely experiences discomfort after great physical exertion or prolonged sitting. The lymphedema remains mild. Consistent wearing of compression garments is certainly partly responsible for the good disease course.

Photograph at the age of 4¾ years. The elongated imprints of the compression garment, which was taken off shortly before the photograph, can clearly be seen on the lower leg. The lymphedema was only mildly pronounced. At this time, the girl had some minor local thrombophlebitis, visible as yellowish circumscribed patches on the skin, similar to a hematoma in regression.

Klippel-Trénaunay syndrome (KTS) is today better referred to as combined capillary-venolymphatic malformation with limb hyperplasia. However, the term KTS is often used to refer very vaguely to a variety of quite different vascular malformations. Even in the presence of KTS in the strict sense, a very good quality of life can be achieved by early, consistent therapy (especially of the lymphatic malformation and the large dysplastic veins), usually with a combination of conservative therapy (compression therapy, exercise therapy) and invasive measures to prevent lymphorrhea or thromboembolic events.
This girl is also expected to have a good prognosis in her long-term course.
Published: 2020
All images © Wohlgemuth