Author(s): Wohlgemuth, Walter A.
Author(s): Wohlgemuth, Walter A.
31-year-old patient with painful, pulsating, hyperthermic mass on the left cheek. This corresponds to a recurrence of a repeatedly pre-embolized and pre-operated arteriovenous malformation (AVM). The overlying skin is discolored reddish.

Typical picture on the overlying skin with infiltration of the cutis by the AVM and a large, increasing mass. In addition to the red discoloration, multiple small teleangiectasias are visible, which are caused by the high venous pressure due to the multiple arteriovenous fistulas. Old scar after previous incomplete resection.

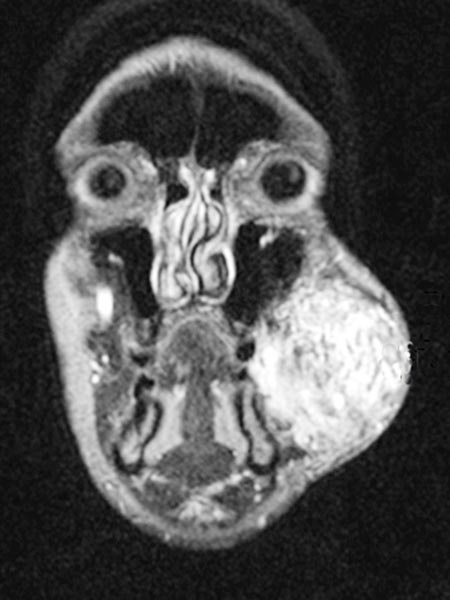
Axial, T2-weighted MRI at the level of the cheek shows the AVM to be relatively hyperintense with edema of the surrounding tissue and extension to the left mandible. In the rostral section some black flow voids are visible as a sign of arteries with fast flow within the AVM.

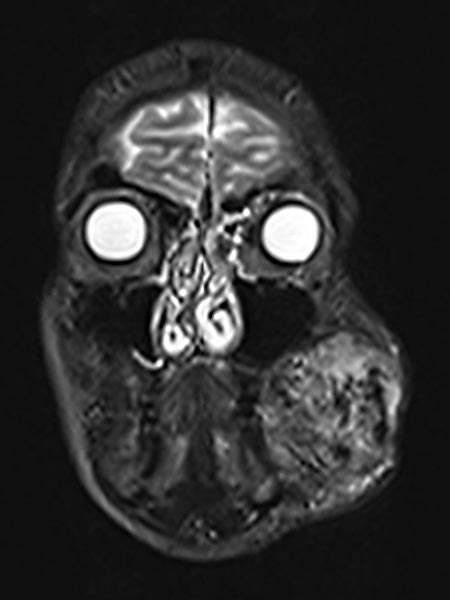
Coronal fat-suppressed T1-weighted MRI after contrast administration shows the inhomogeneous marked enhancement of the AVM. This is typical of an AVM in the stage of proliferation (corresponding to rapid enlargement) and correlates well with the edema in the T2-weighted images.
Coronal T2-weighted fat-saturated MRI showing hyperintense edema within the AVM and flow voids due to fast-flow arteries.
Inhomogeneous, peripheral enhancement of the proliferating AVM in this axial fat-suppressed T1-weighted MRI after contrast administration. No circumscribed component that is actually solid, unlike in a true vascular tumor.
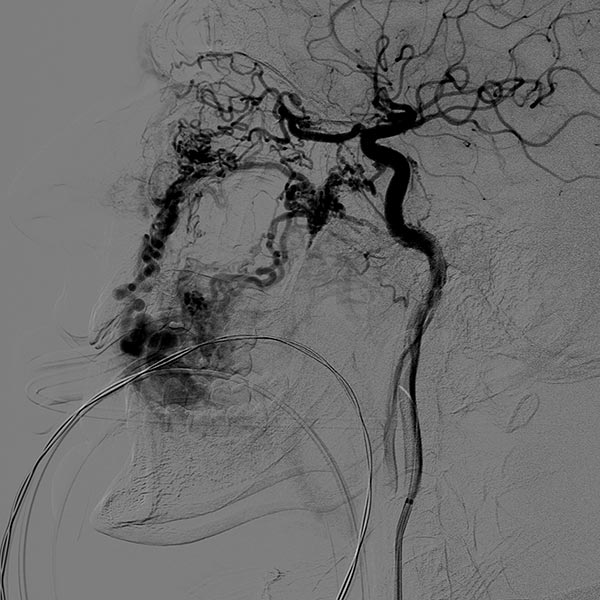
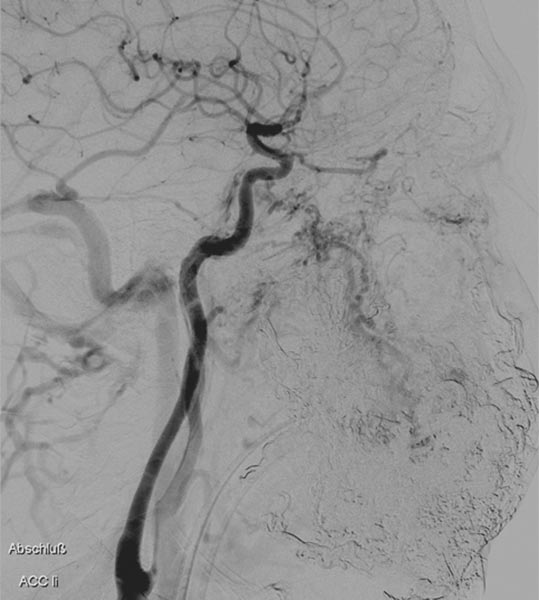
Lateral view of a digital subtraction angiography after contrast injection into the left external carotid artery. The AVM is visible as a diffuse, reticular net-like nidus with direct, strong venous outflow centrally in the left cheek (fast-flow malformation).
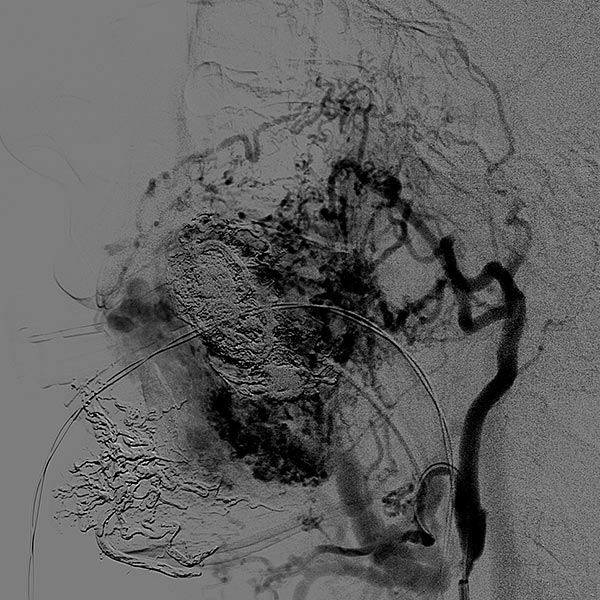
Lateral view, DSA after contrast injection in the left internal carotid artery. There is also a massive supply to the nidus of the AVM from the internal carotid artery, mainly via the ophthalmic artery and the meningohypophyseal trunk.
This complicates embolization therapy considerably.
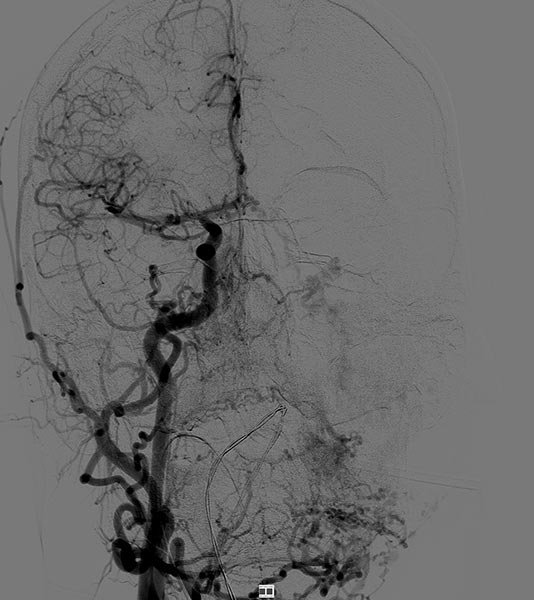
DSA, anterior-posterior view, after injection into the right common carotid artery. The nidus of the AVM on the left cheek is also supplied from the contralateral right external carotid artery and right facial artery.
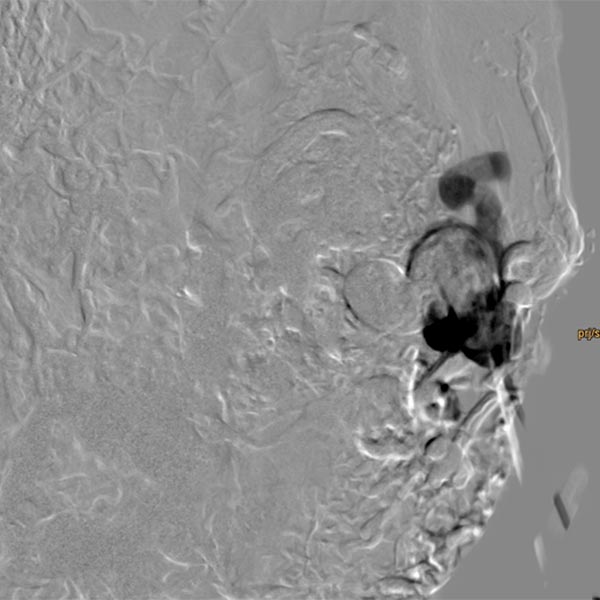
Direct percutaneous puncture of the nidus with a needle in DSA. This direct contrast injection is necessary to verify the correct position of the needle tip before embolization using ethylene-vinyl alcohol copolymer in a direct puncture technique.
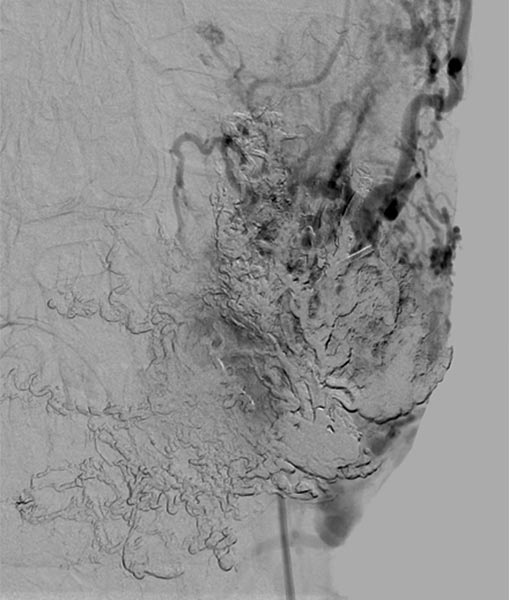
Renewed direct puncture of the nidus and DSA to check needle position.
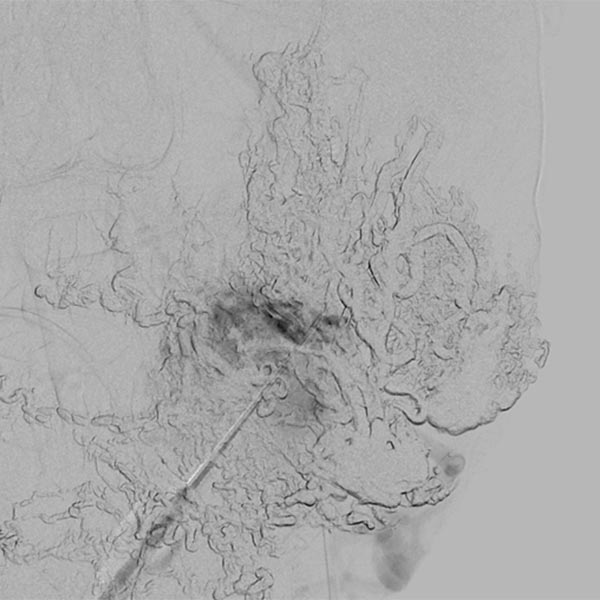
Slow, direct filling of the nidus and draining veins using ethylene-vinyl alcohol copolymer (EVOH) in roadmap technique. Already pre-injected EVOH is subtracted away in this technique and is only visible in outline.
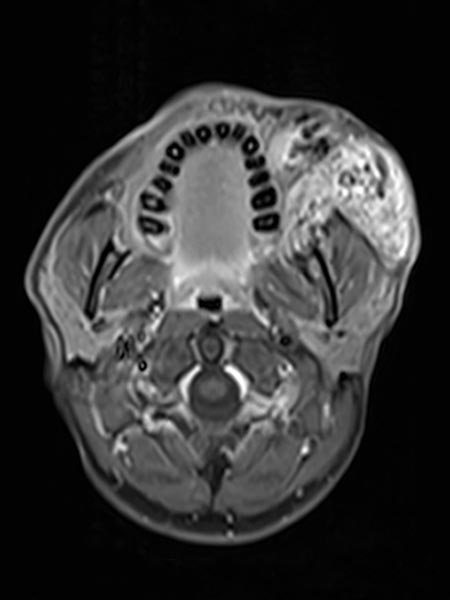
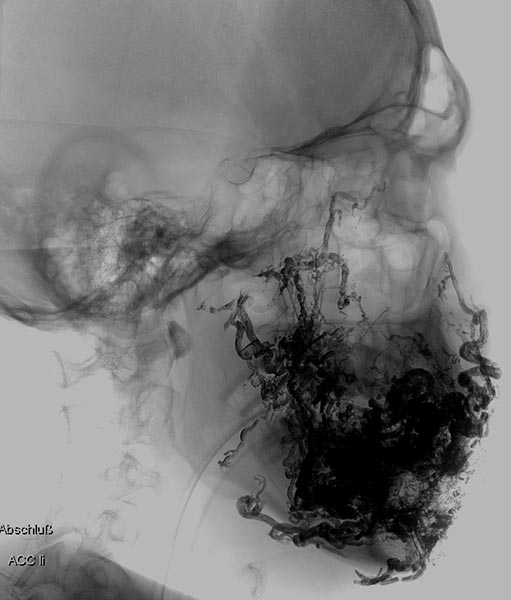
Complete filling of the entire nidus of the AVM using ethylene-vinyl alcohol copolymer (EVOH). This is visible in the radiograph shown here (AP) as a black, reticular radiopaque cast specimen within the occluded AVM vessels.

Filling of the entire nidus of the AVM using ethylene-vinyl alcohol copolymer, which is visible in the radiograph shown here (lateral view) as a black, reticular radiopaque cast within the occluded AVM vessels.
Late phase of DSA (lateral view) via the left internal carotid artery. After successful multiple embolizations, the supply to the nidus of the AVM via these critical branches is also occluded and the ophthalmic artery is preserved.
As a result of the extensive embolization, a small mucosal wound occurred on the left lower lip one week after the last embolization. A small piece of the embolized ethylene-vinyl alcohol copolymer emerged from this. The wound healed after 3 weeks without complications. Otherwise, no skin necrosis or ischemia occurred, and the facial nerve is preserved.
![[Translate to Large arteriovenous malformation of the cheek:] Große arteriovenöse Malformation an der Wange Small mucosal wound occurred on the lower lip](/fileadmin/images/patientenbeispiele/4-avm-wange/f04-16-embolisat-lippe-avm.jpg)
Intraoperative image of the site during resection of the occluded nidus (Prof. Reichart, Regensburg University Hospital). Step-by-step microsurgical preparation of the completely embolized nidus, which penetrates the entire cheek. To preserve the facial nerve, neuromonitoring of the facial branches is performed during the entire preparation, visible here from several needle electrodes at the right of the image.
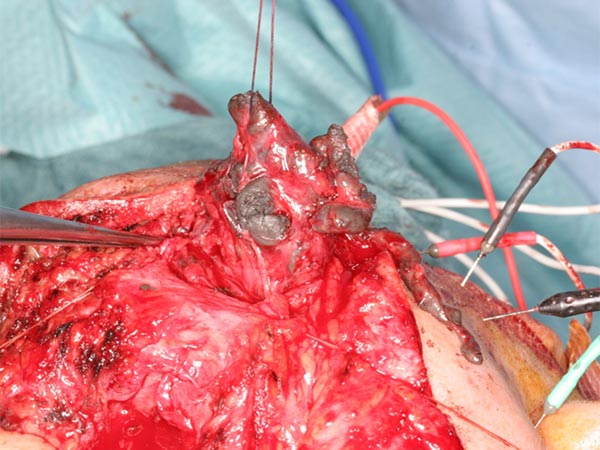
Resected specimen of the nidus of the AVM. This is deep red due to the many blood vessels of the AVM and contains multiple black vascular structures due to the embolic agent ethylene-vinyl alcohol copolymer (cast).
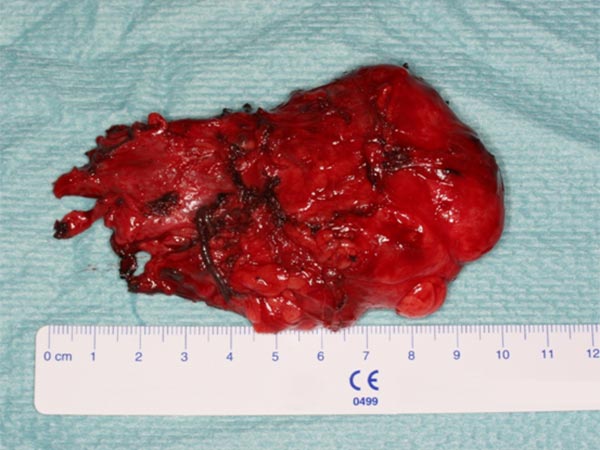
In a second resection, any remaining residual embolized nidus was resected to allow for the most radical removal possible to avoid recurrence. Note the abundance of vessels (deep red) and the black embolization material in the occluded nidus.

Closure of the skin access during the second operation, also with neuromonitoring. As blood flow was now greatly reduced, the skin redness has regressed.

Development before and after treatment. Photograph immediately before treatment.

Development before and after treatment. Photograph after the treatment series involving 3 embolizations and 2 resection operations of the then occluded nidus of the AVM.

After successful combined therapy (complete embolization + resection of the occluded nidus) with preservation of the facial nerve, the mass effect of the AVM is also eliminated. The patient is free of recurrence 4 years after the procedures (photograph). The skin redness has regressed. However, he must continue to be clinically monitored so that late recurrence can be detected and treated, if necessary.

Large, infiltrating, often incompletely or inadequately treated facial arteriovenous malformations (AVM) are particularly difficult to treat. The arterial feeders are supplied from all supra-aortic branches in the long-term course, and progression is rapid and penetrates all tissue layers.
Embolization of even small branches from the internal carotid artery is technically demanding and carries risk, as does complete occlusion of the nidus. Subsequent resection of the occluded nidus is equally difficult because the facial nerve is often directly embedded in the nidus. Intraoperative neuromonitoring to preserve the facial nerve is helpful here.
Since recurrence cannot be reliably ruled out in the long-term course even with a radical procedure, long-term follow-up is necessary. In view of the large arteriovenous malformation in this localization, the patient’s progress so far is very encouraging.
Published: 2018
All Images © Wohlgemuth












![[Translate to Large arteriovenous malformation of the cheek:] Große arteriovenöse Malformation an der Wange Small mucosal wound occurred on the lower lip](/fileadmin/_processed_/9/a/csm_f04-16-embolisat-lippe-avm_d7e489a8e9.jpg)







