Author(s): Wohlgemuth, Walter A.
Author(s): Wohlgemuth, Walter A.
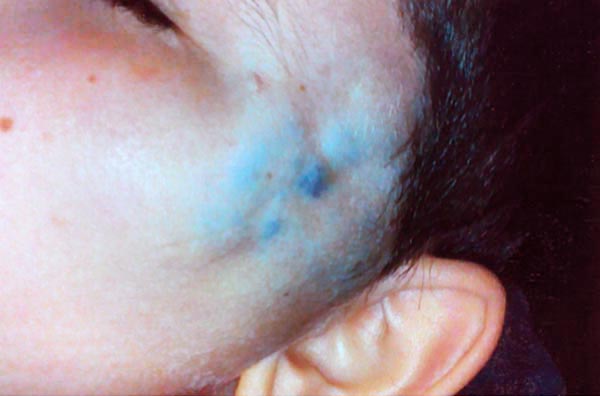
9-year-old boy with a soft, bluish swelling in the left preauricular position, suspected venous malformation.
No increase of the swelling during physical exertion and Valsalva maneuvers, therefore glomuvenous malformation possible. Small scar from an unsuccessful previous operation.
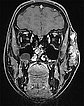
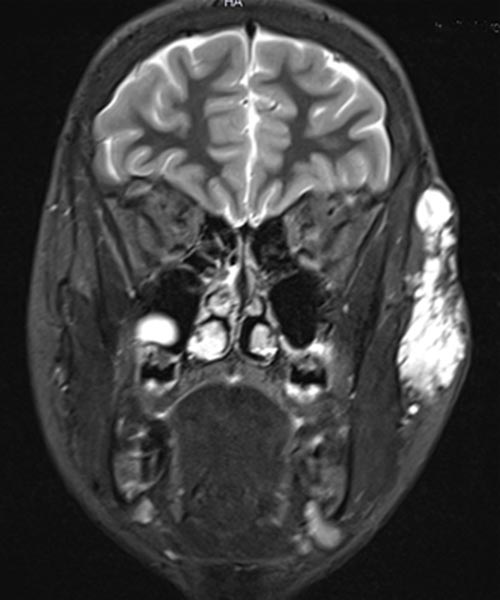
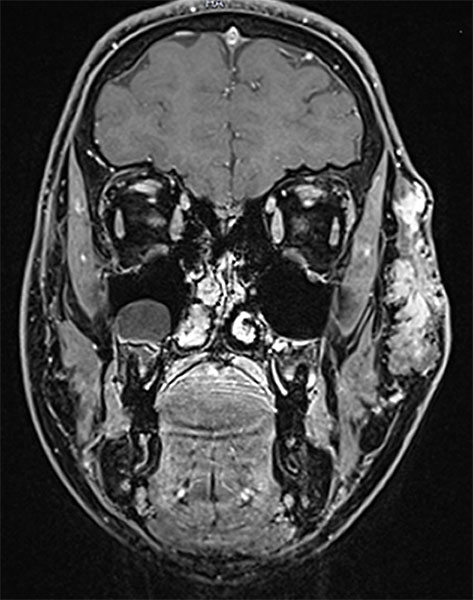
Coronal, T2-weighted fat-suppressed MRI of the face. The venous malformation typically appears very hyperintense (white).
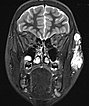
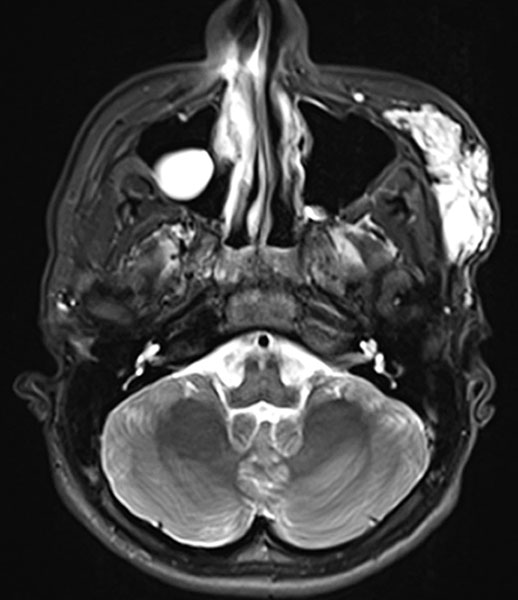
Axial, T2-weighted fat-suppressed MRI of the face. The venous malformation appears typically very hyperintense here too. No expansion into the depth.
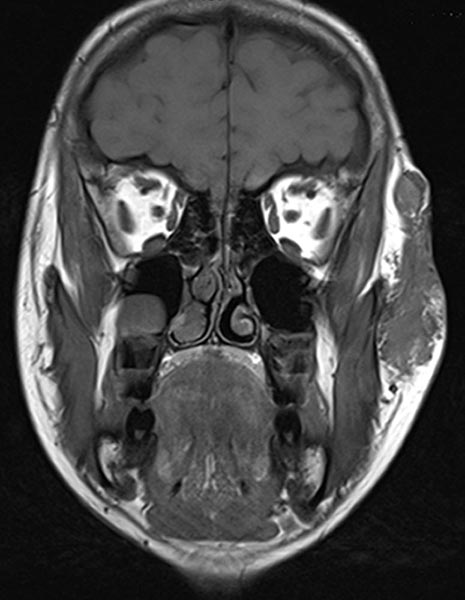
Coronal, T1-weighted MRI of the face. The venous malformation appears isointense to the musculature and is embedded in the surrounding fatty tissue.
Coronal, contrast-enhanced, dynamic MR angiography, MIP imaging 33 s after injection of the contrast medium. The contrast dynamic is in the venous phase, the venous blood vessels are fully contrasted. The venous malformation itself does not accumulate any contrast medium at this time.

Coronal, contrast-enhanced, dynamic MR angiography, MIP displayed 124 s after injection of the contrast agent, thus a late venous phase. Only now does the venous malformation slowly accumulate some of the contrast medium (“pooling”).

Coronal, T1-weighted fat-suppressed MRI of the face after administration of contrast medium. The venous malformation enriches the contrast medium more clearly after 4 minutes, but relatively slowly and not yet completely at the time of imaging.
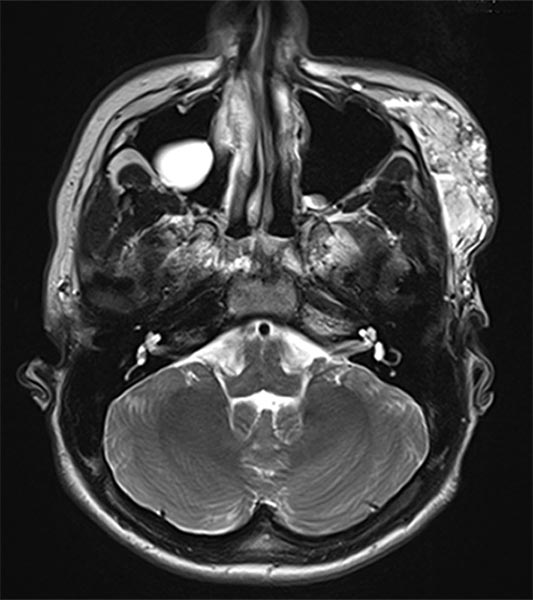
Axial, T2-weighted MRI of the face (without fat suppression). The venous malformation is highly hyperintense and shows fluid-fluid levels.
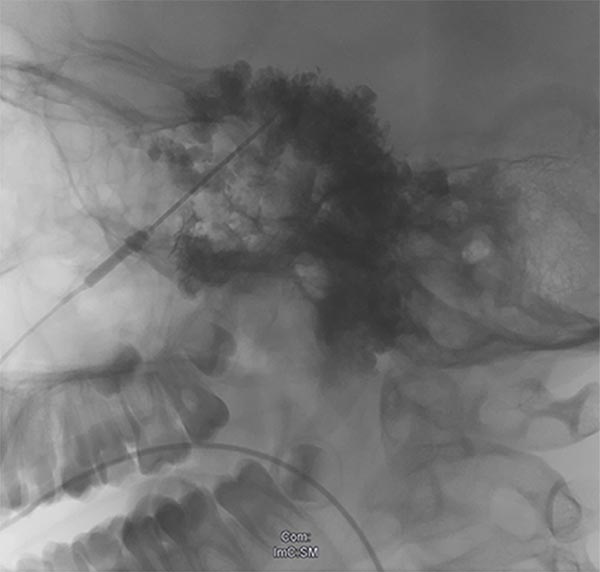
X-ray after direct injection of contrast medium into the venous malformation via 2 puncture needles. No outflow via any communication veins, good needle position for sclerotherapy. Now 2 ml of Aethoxysklerol 3% 1:4 admixed with air (foam sclerotherapy) are injected.

X-ray after injection of contrast medium into the venous malformation during the 2nd sclerotherapy 8 months later. Again no outflow via communicating veins is displayed. Good needle position for another foam sclerotherapy (3 ml Aethoxysklerol 3%, foamed 1:4 with air).
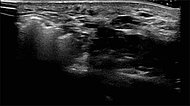
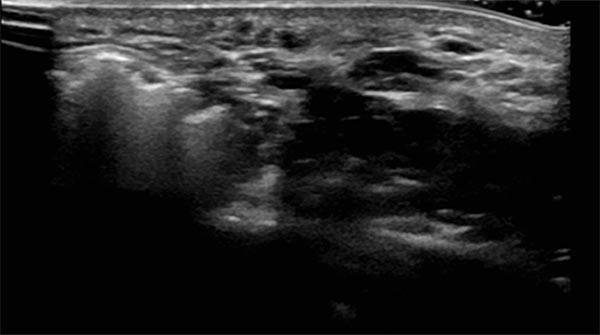
Sonography during sclerotherapy treatment. At the right side of the picture the still unfilled parts of the venous malformation, shown black as nearly echo-free vascular channels. On the left side lesion already filled by the sclerosing foam, echogenic with dorsal acoustic shadowing.
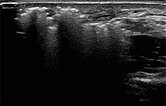
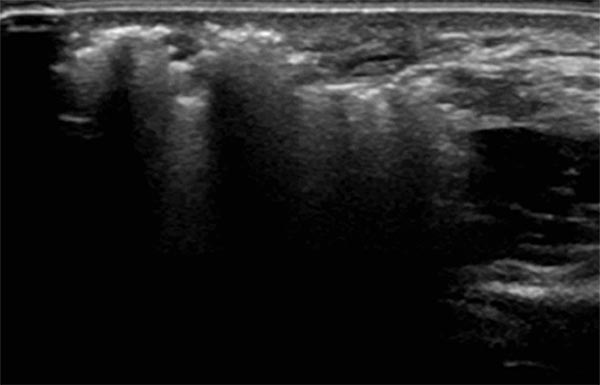
Sonography during sclerotherapy treatment. Now further filling of the venous malformation by the sclerosing foam. When the entire malformation is filled with the foam, the injection can be terminated.
After the second sclerotherapy, the swelling and discoloration were already significantly improved. The patient was largely free of complaints.

X-ray after injection of contrast medium into the venous malformation, for what is now the third sclerotherapy treatment after pain recurrence. Almost the entire remaining venous malformation is contrasted by contrast injection at the current needle position. Now 4.5 ml of Aethoxysklerol 3%, foamed 1 to 4 with air, is injected.

After the third sclerotherapy, swelling or discoloration have vanished. The patient is free of complaints. The photograph 7 years later of the patient, now 16 years old, proves that he is free of recurrence.

Venous malformations (VM) are particularly common in the facial area. Recurrent thrombophlebitis caused by coagulation processes within the blood-filled, dysplastic vascular spaces leads to pain. The esthetic appearance of the visibly discolored and swollen lesion in the face must be considered.
With a low-risk sclerosing treatment, here in the form of foam sclerotherapy, the venous malformation usually cannot be completely removed, but it can be greatly reduced. The swelling decreases. In addition, the patient becomes asymptomatic, as clots no longer form in the closed vascular spaces.
Published: 2018
All images © Wohlgemuth