Author(s): Wohlgemuth, Walter A.
Author(s): Wohlgemuth, Walter A.
Female patient 8 years of age at the time, with elongated left leg (leg length discrepancy +1.8 cm), which is always significantly warmer than the right leg. In the left lower leg, ankle and foot there is permanent slight edema, here in the form of phlebedema due to the increased venous pressure with extensive arteriovenous fistulas of the entire left lower extremity. Purpura jaune d'ocre as deposits of erythrocytes in the skin due to red blood cells being squeezed out in chronic venous hypertension.

The marked phlebedema of the left leg with swelling in the distal region in chronic venous hypertension due to the multiple arteriovenous fistulas is clearly seen when comparing sides.

The picture at 12 years of age shows progression of both skin manifestations and edema. Owing to the accompanying progressive hyperplasia of the left lower extremity, it also appears significantly larger than the right side in terms of soft tissue.

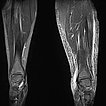
Composite T1-weighted coronal MRI from the pelvis to the feet. Not only the leg length discrepancy (osseous hyperplasia) is clearly visible, but also the significantly larger musculature on the left side and the enlarged adipose tissue. The hyperplasia of the extremity affects all tissues in Parkes-Weber syndrome.
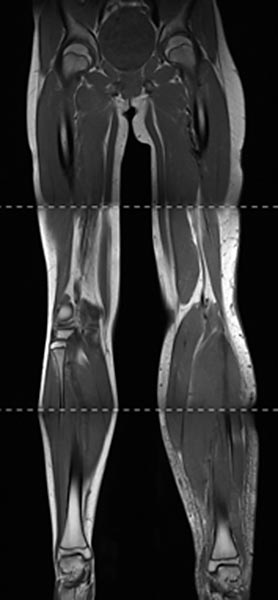
Coronal, T2-weighted, fat-suppressed MRI of both lower legs. Marked subcutaneous edema on the affected left side due to chronic venous hypertension.
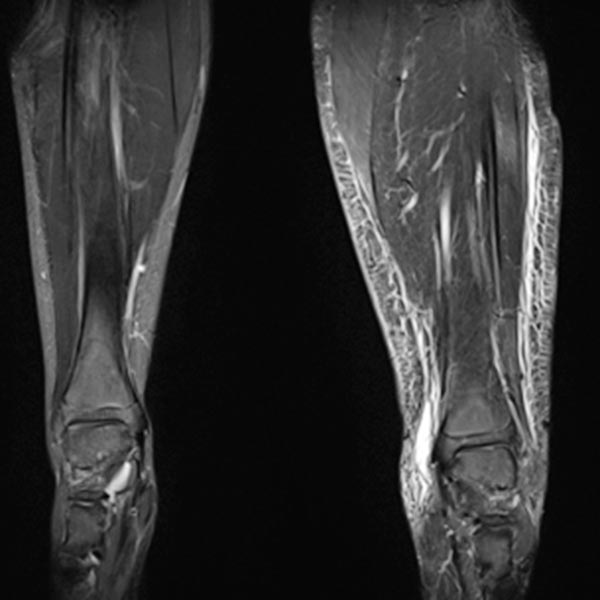
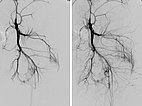
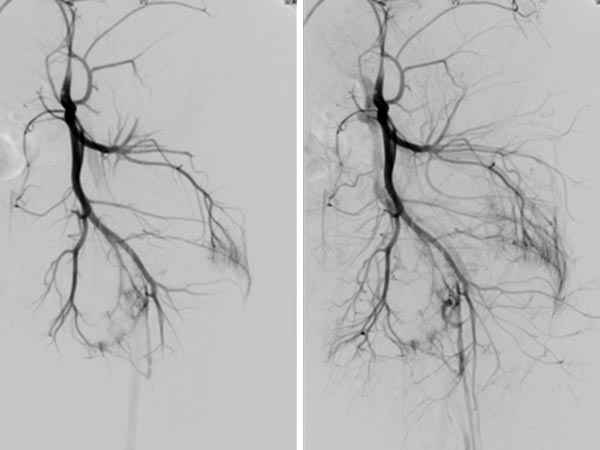
MIP reconstruction of a contrast-enhanced dynamic MR angiography of the pelvis and thighs. While an arterial phase is still present on the normal right side, the arteries and veins of the left side are massively dilated and already contrasting the draining veins because of the multiple arteriovenous fistulas seen in Parkes-Weber syndrome.

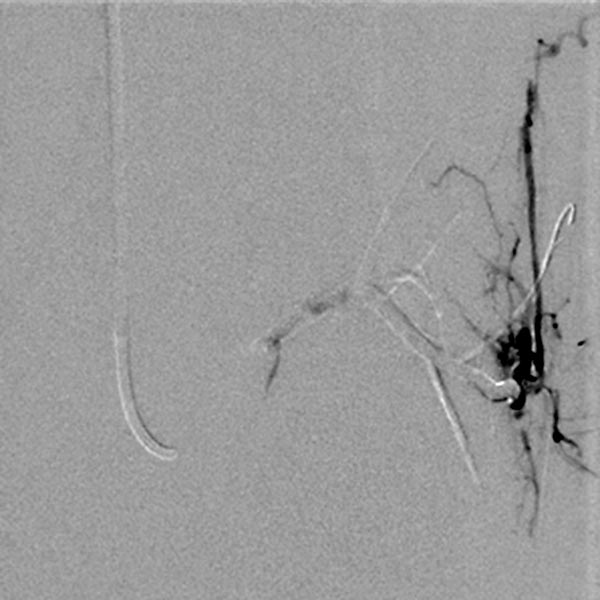
Digital subtraction angiography, with the catheter in the left superior gluteal artery, reveals multiple, barely identifiable small arteriovenous fistulas typical of the diffuse arteriovenous malformations seen in Parkes-Weber syndrome.
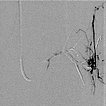
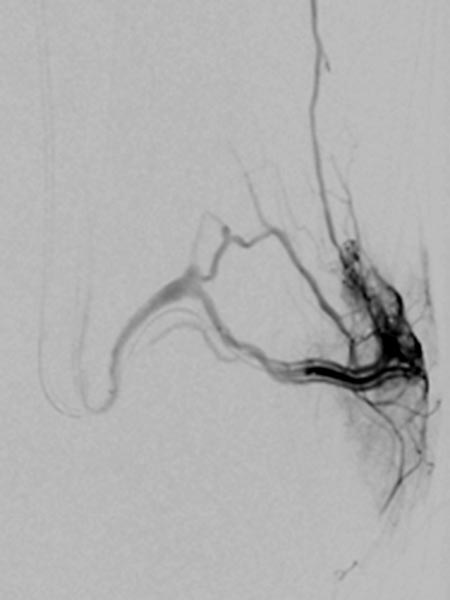
Superselective digital subtraction angiography via a microcatheter in the superior gluteal artery in a distal branch. The nidus of the fine fistulous arteriovenous malformation shows such fine shunts that they can hardly be resolved anatomically on angiography.
During embolization via the microcatheter (not shown) using the roadmap technique, the embolic agent (ethylene-vinyl alcohol copolymer) is pushed forward into the nidus and further into the venous outflow of the AVM to close even the smallest fistulas ("plug & push" technique).
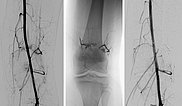
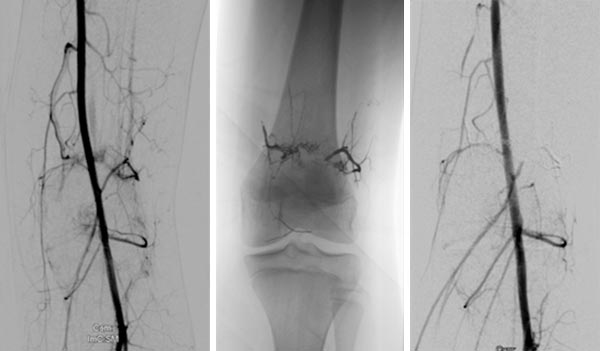
Further stepwise embolization of the main areas of the arteriovenous malformation, here at the knee. The cast specimen caused by the radiopaque embolization material (ethylene-vinyl alcohol copolymer) shows the occlusion down to the smallest vessels.

DSA before embolization (left) shows multiple fine AVMs near the knee joint. In the non-subtracted radiograph after embolization, the radiopaque embolic agent can be seen (middle), completely filling the arteriovenous fistulas. In DSA after embolization (right), the entire nidus of the AVM is occluded, no more arteriovenous fistulas are visible.
Photograph now in the 13th year of life. The edema is somewhat less pronounced after the embolizations because the venous pressure is lower. Nevertheless, the purpura jaune d'ocre has increased. Its color change is also typical, from proximally paler and redder to distally darker and more color-intensive due to the distally higher hydrostatic pressure, which leads to more erythrocytes being squeezed out of the venous system.

This disease course in a child with Parkes-Weber syndrome shows some typical characteristics of the clinical picture. It diffusely affects an entire limb and shows multiple, very fine fistulous arteriovenous fistulas in the sense of an extensive arteriovenous malformation (AVM). Concomitantly, the affected limb is not only enlarged due to edema from the increased venous pressure, but there is also concurrent true hyperplasia of all tissues of the affected limb. Extensive embolization is indicated when venous pressure becomes too great and significant discomfort or marked skin manifestations occur. In addition, temporary epiphysiodesis is often necessary in children due to progressive leg length discrepancy. Before insertion of the staples or "eight-plates" for temporary growth inhibition, the parts of the AVM close to the knee joint must be occluded, as was the case in this patient, in order to allow the osteosynthesis material to be inserted and removed without complications and blood loss.
Despite successful embolization and epiphysiodesis, this girl will also have to wear compression garments permanently on the affected leg, since the entire AVM can never be occluded because of its extension.
Published: 2020
All images © Wohlgemuth