Author(s): Wohlgemuth, Walter A.
Author(s): Wohlgemuth, Walter A.
Photograph of the boy, then 7 years old, with slowly progressive, clearly painful swelling laterally at the level of the right knee joint. A distinct pulsation is felt on palpation. Genetically confirmed PTEN hamartoma syndrome.

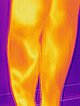
Infrared thermographic photograph of the swelling laterally at the level of the right knee joint shows marked local hyperthermia (yellow-white), indicative of significant arteriovenous shunts of an AVM.

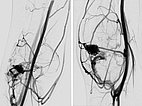
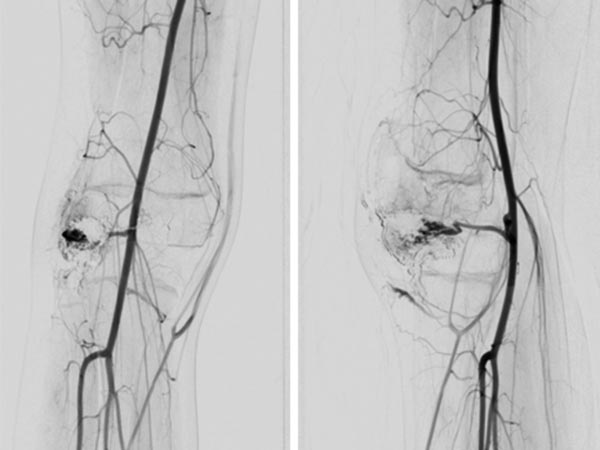
Digital subtraction angiography (DSA) of the knee (left AP projection, left lateral projection) shows an AVM with a rather spherical, aneurysmal nidus as well as another nidus intraosseously in the lateral tibial plateau. This very spherical, aneurysmal nidus together with the painful, progressive mass is suggestive of a PTEN hamartoma.
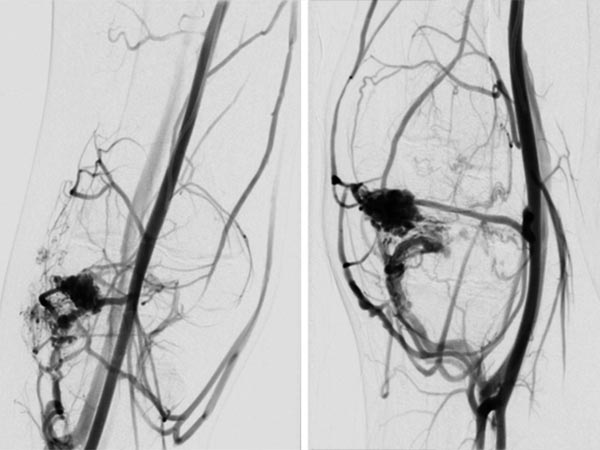
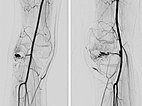
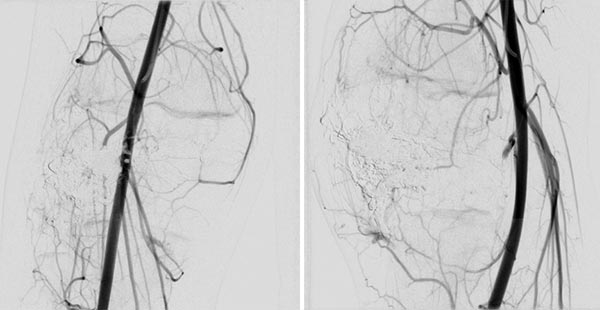
After successful embolization of the two AVM nidus parts, the radiographic overview images (left AP, right lateral projection) shows a complete cast specimen of the two portions caused by the embolic agent, the so-called cast. This consists of ethylene-vinyl alcohol copolymer, which contains radiopaque tantalum.
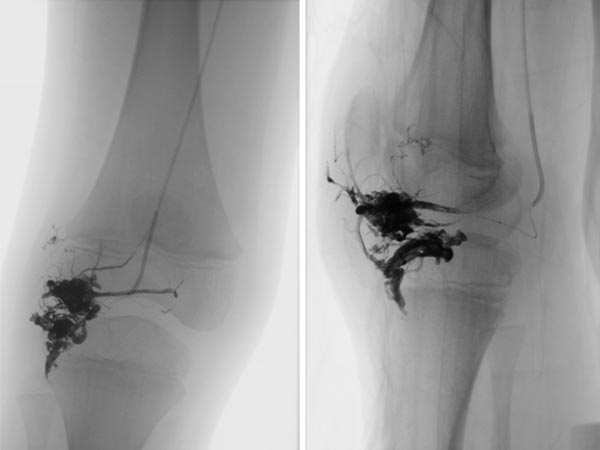
In the control DSA (left AP, right lateral) after embolization with ethylene-vinyl alcohol copolymer, no more perfusion is seen in the angiography even in a long series. The AVM is considered to be occluded.
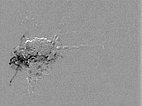
The repeat DSA 4 months after the previous embolization (left AP, right lateral) shows an early, circumscribed recurrence. Especially in the case of AVMs associated with a PTEN hamartoma syndrome, patients must attend for follow-up at short intervals, as these AVMs in particular have a high tendency to recur.
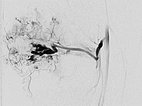
After renewed superselective catheterization of the AVM-feeding artery (lateral inferior genicular artery) ), the microcatheter is advanced to just before the nidus.
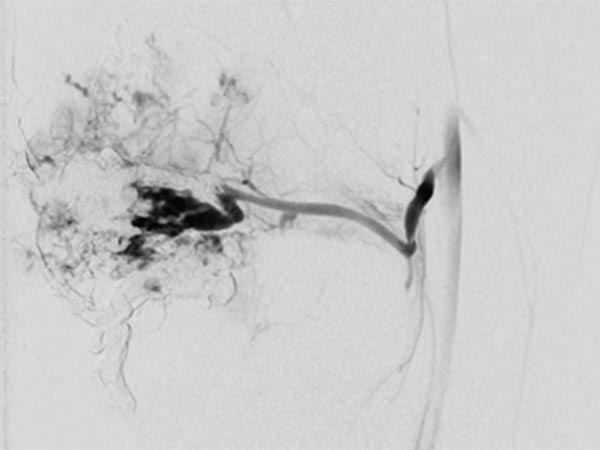
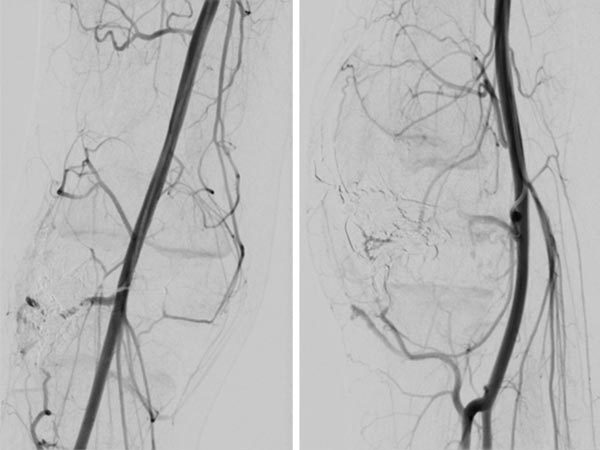
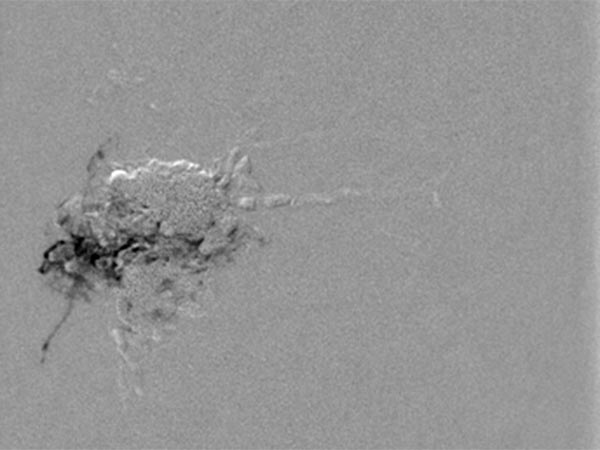
DSA image (roadmap technique) during re-embolization shows the freshly injected new additional embolic agent as black in the image.
Final DSA images (left AP, right lateral projection) after completion of repeat embolization again shows angiographically complete occlusion of both portions of the AVM.
Photograph immediately after the last embolization. The local mass caused by the PTEN hamartoma with the contained AVM has increased in size. Embolization is now complete, so that the lesion can now be resected.

Photograph of patient 3 months after successful resection of completely embolized PTEN hamartoma.

Infrared thermography image postoperatively shows no more heating in the area of the right knee, nor any remnants or recurrence after embolization.
Here the warmer areas are color-coded yellow to whitish.

PTEN hamartoma syndrome is often diagnosed after a delay. Multiple arteriovenous malformations (AVM), which angiographically appear to include a spherical aneurysm, and a clear accompanying painful soft tissue lesion are often indicative. If this is accompanied by dilated head circumference, a PTEN mutation may be the reason. Early recurrence is common after embolization of these AVMs, and resection of the occluded nidus should be attempted whenever technically possible. This was also the plan in this patient. The recurrence occurred early after the first, angiographically complete embolization. After repeat embolization, the extraosseous portion of the nidus was then successfully resected. The intraosseous portion in the tibia shows no recurrence at follow-up to date.
Published: 2020
All images © Wohlgemuth