Author(s): Wohlgemuth, Walter A.
Author(s): Wohlgemuth, Walter A.
At the age of two years and one month, a small, clearly painful swelling formed for the first time in a previously completely inconspicuous, medial supraclavicular area on the left side of the neck. At that time there was small induration in the sense of acute thrombophlebitis within the venous malformation. The volume of the swelling fluctuated up to the time of the clinical presentation eight months later, sometimes slightly larger, sometimes slightly smaller. However, the overall volume increased markedly over the months. The overlying skin shows minimal bluish discoloration.

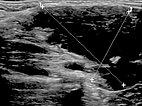
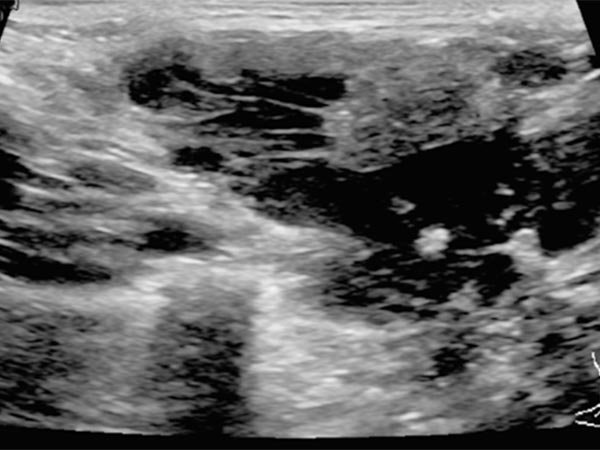
B-scan ultrasonography (longitudinal section) shows the venous malformation to be relatively homogeneously hypoechoic to anechoic. The venous dysplastic vascular channels are compressible with the ultrasound transducer and contain liquid blood.
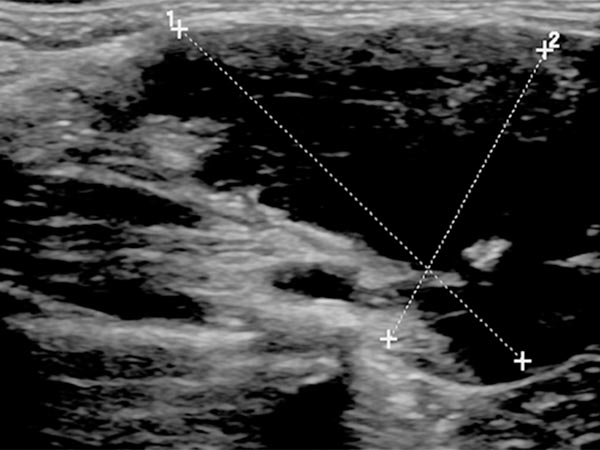
B-scan ultrasonography (cross-section) also shows the venous malformation as combined hypoechoic to anechoic. The more echogenic parts correspond to sections of the venous malformation in which the contained blood has already clotted. In the anechoic portions, the contained blood is still liquid. In addition, a small phlebolith is found in the lesion, which is practically pathognomonic for a venous malformation.
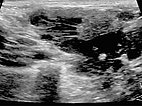
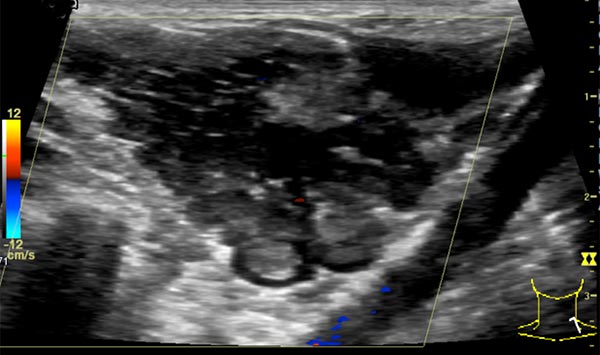
In color-coded duplex sonography, the venous malformation is also clearly delineated. Because it is a slow-flow lesion, it shows virtually no perfusion here. Flow through the lesion is minimal. Very few color signals are found outside the venous malformation, despite the selection of low pulse repetition frequency.
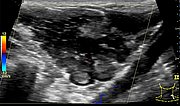
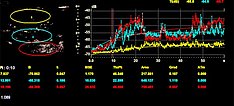
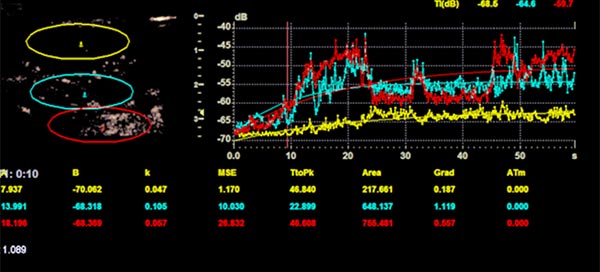
In quantitative contrast-enhanced sonography (CEUS), several areas of interest are continuously measured with regard to their contrast enhancement for perfusion analysis of the venous malformation. The values measured here also show the classic character of a slow-flow lesion.
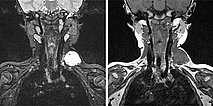
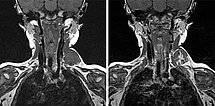
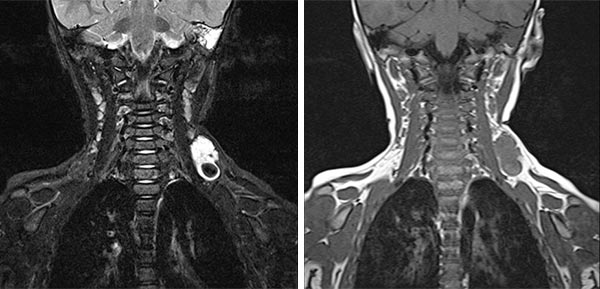
In coronal MRI (left image: T2-weighted, right image: non-enhanced T1-weighted), the venous malformation (VM) is very well delineated. It is strongly hyperintense in the T2 image, whereas it is isointense to the musculature in the non-enhanced T1 image. The signal intensity is typical of the character of a slow-flow lesion.
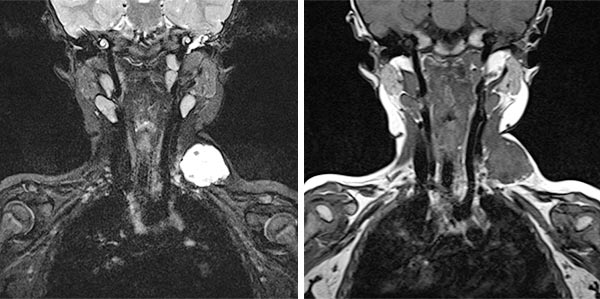
In coronal MRI (left: T2-weighted, right: T1-weighted non-enhanced) slightly more dorsally, a larger thrombus within the venous malformation is very well delineated. In the T2 image, this is hypointense compared to the severely hyperintense venous malformation. In the non-enhanced T1 image it is slightly more hyperintense than the surrounding hypointense venous malformation.
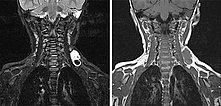
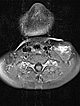
Axial MRI (T2-weighted) also shows the dorsal location of the larger hypointense thrombus within the severely hyperintense venous malformation. In addition, a classic fluid-fluid level within the venous malformation is depicted. The heavier corpuscular components with somewhat lower signal intensity settle dorsally with gravity (dorsal position), the liquid blood serum with somewhat higher signal intensity "floats" up (ventral position), and a fluid-fluid level forms in between.
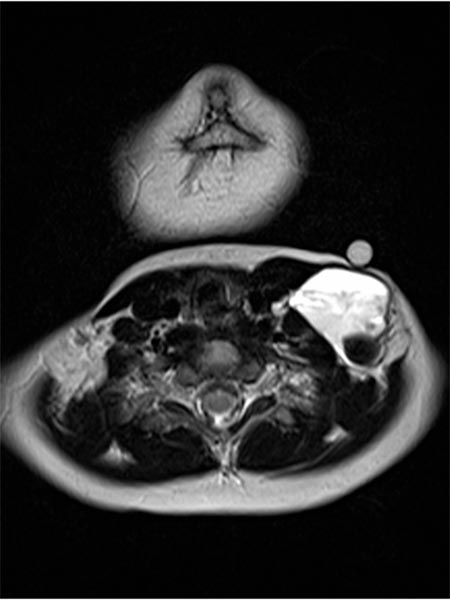
Axial MRI (T1-weighted) at the same level after contrast administration shows central enhancement within the venous malformation. However, this enhancement is relatively slow (“pooling”) and detectable only minutes after contrast injection and is still incomplete at the time of imaging.
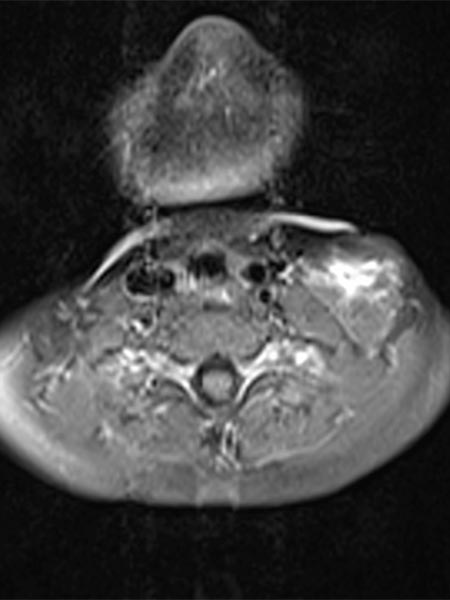
Coronal MRI, T1-weighted, left image before and right image after contrast administration, on the same slice plane very clearly shows the inhomogeneous contrast uptake, which is still incomplete at this time. The lesion slowly takes up contrast from central to peripheral in a radial fashion.
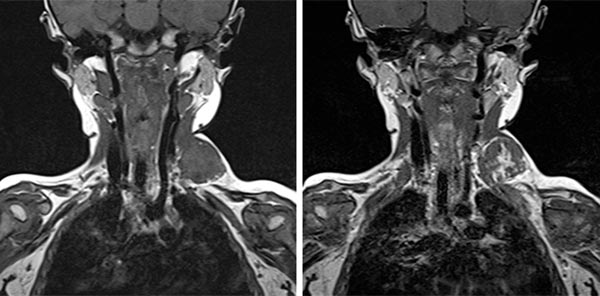
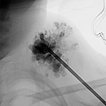
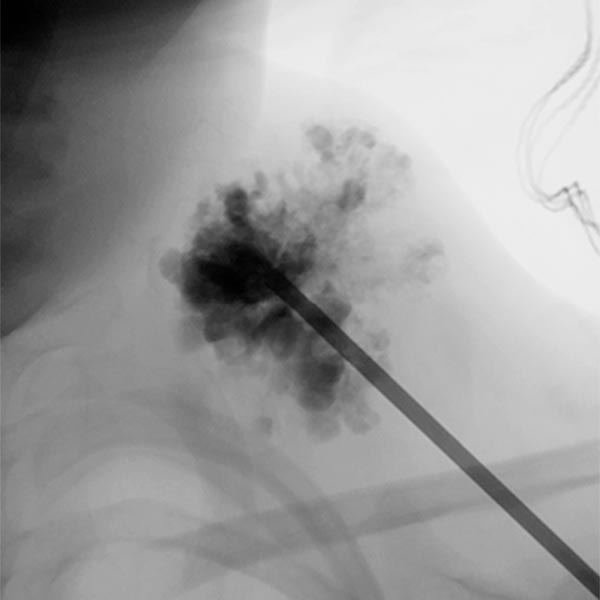
Sclerotherapy was performed in view of the rapid growth in size and recurrent painful thrombophlebitis. The contrast injection via an inserted puncture needle depicted here shows extensive contrasting of the venous malformation, thus good conditions for successful sclerotherapy.
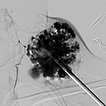
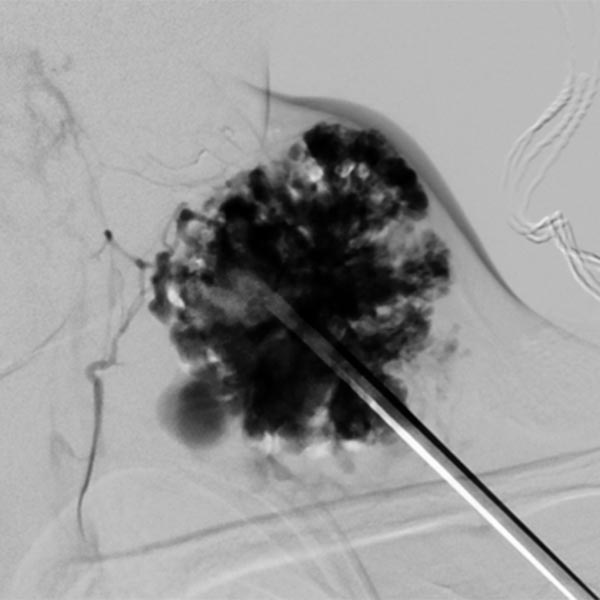
Digital subtraction angiography after contrast injection via the same needle also shows very clearly the almost complete filling of the venous malformation from this needle position. Only small, very thin-lumen communicating veins present themselves. Therefore, a large part of the venous malformation can be sclerosed from this needle position.
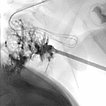
In the fluoroscopic control (lateral plane) after injection of 8 ml of polidocanol foam (3%, 1 : 4 foamed in air), the entire venous malformation is filled with the non-contrasting foam. The previously contained contrast medium is almost completely displaced by the sclerosing foam. Thus there is a good chance that the lesion will be very largely closed by the procedure.
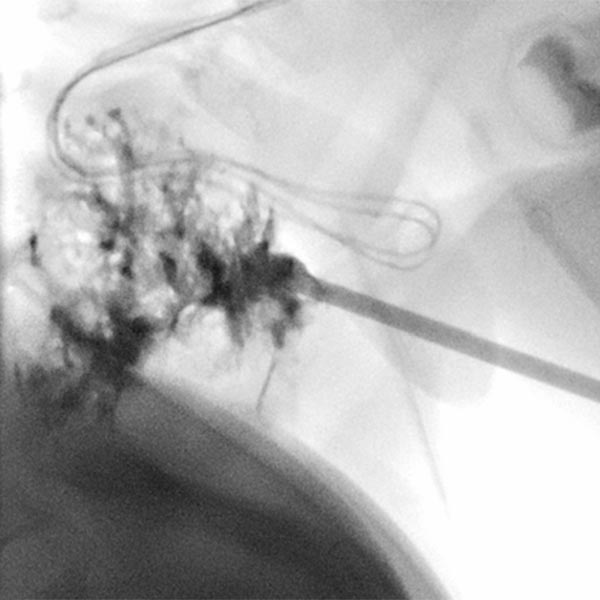
Circumscribed venous malformations (VM) may remain asymptomatic for a long time and cause few problems, depending on the anatomic location and tendency to progress. In a minority of patients, however, a marked tendency to increase in size is present as early as infancy. These lesions often become symptomatic through localized space-occupying swellings (usually with painful thrombophlebitis). Invasive therapy, either by sclerotherapy or open resection, will then be indicated even in infancy. In the case presented here, the child was successfully treated by a total of two sclerotherapy sessions, in this case foam sclerotherapy with polidocanol foam. Both the local space-occupying effect and the recurrent thrombophlebitis no longer occurred.
Published: 2018
All images © Wohlgemuth